Medicine in Psychiatry Services (MIPS)
Our Mission
MIPS aims to be:
- a community leader for comprehensive healthcare targeted to patients with concomitant medical conditions and psychiatric illnesses, including substance use disorders
- a national center of innovation, education and research focused on integrating medical, psychiatric and social services.
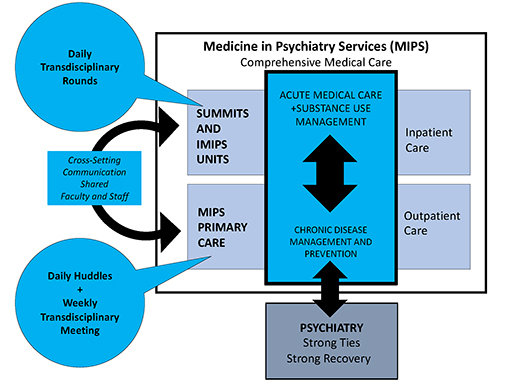
Healthcare innovation is needed to address the significant health disparities faced by patients with psychiatric conditions. The University of Rochester’s department of Psychiatry is unique in that it has its own division of Medicine in Psychiatry Services (MIPS) to address the often under-recognized medical needs of psychiatry patients.
MIPS division faculty members are trained in family medicine and internal medicine and come with expertise in primary and acute medical care. Some have additional training in addiction medicine, mental health or geriatrics.
All are actively involved in education and quality improvement initiatives to improve medical care for patients with medical and psychiatric conditions.
MIPS clinical services include a patient-centered primary care medical home and two acute medicine units (30 beds) for adults with medical conditions and concurrent psychiatric conditions.
Patient Care
We are committed to interdisciplinary collaboration and partnering with patients and their families to provide care that is accessible and individualized.
IMIPS
Our specialized inpatient unit works closely with the MIPS Primary Care Team to provide high-quality, compassionate care for hospitalized patients with acute medical conditions.
SUMMITS
A one-of-a-kind hospital unit committed to providing acute medical care to people who have substance use disorders that need extended hospital treatment.
MIPS-PC
This national model provides primary medical care alongside behavioral health and chemical dependency treatment, offering integrated care to individuals at high risk for chronic diseases.
Innovations in MIPS
The department of Psychiatry is unique in that it runs its own specialized medical services provided by a team of nurses, nurse practitioners, physician assistants, and physicians who provide acute hospital-based and primary medical care.
MIPS provides:
- Acute medical care to adults in two specialized medicalunits:
- The Inpatient Medicine in Psychiatry (IMIP) unit
- The Substance Use Medical Management, Infection Treatment and Support (SUMMITS) unit
- Medical evaluation and consultation to adult patients admitted to the inpatient psychiatric units
- Primary medical care for patients who are part of the MIPS clinic
- Close collaboration with social workers, pharmacists, peer-specialists, psychiatrists, psychologists and counselors
Clinical Innovations
Learn more about the innovative medical care in our units and primary care office.
Education and Training
MIPS is a required rotation for University of Rochester psychiatry residents in their first year, and an elective rotation for University of Rochester internal medicine residents, who can also choose to participate in the Medicine in Psychiatry Track, which provides longitudinal training and scholarship opportunities in MIPS.
MIPS is also popular for elective rotations among medical students, nursing students, family medicine residents and other trainees from the University of Rochester and nearby institutions.
MIPS educational opportunities:
Our Research
Many faculty and staff in the MIPS division are actively involved in clinical research related to the MIPS mission. Below are examples of important ongoing and previous research.
Laboratory of Integration Services for Complex Needs (LISCN) seeks to study patient’s needs and priorities across the biomedical, psychiatric and social spheres and develop innovative solutions for integrated care.
Recent Publications
Padrino, S., Chan, A. C., van Schijndel, M., & Wittink, M. (2024). Medical Psychiatry Units: a Delphi consensus approach to defining essential characteristics. Journal of the Academy of Consultation-Liaison Psychiatry.
https://doi.org/10.1016/j.jaclp.2024.09.004
Choi, J. J., Maeng, D. D., Wittink, M. N., Olivares, T. E., Brazill, K., & Lee, H. B. (2024). Enhanced Primary Care for Severe Mental Illness Reduces Inpatient Admission and Emergency Room Utilization Rates. Population Health Management.
https://doi.org/10.1089/pop.2024.010
Gensler, L.,Kim, S.; Pinto, C.,Padrino, S., Wittink, M. (September 20, 2024) Medical Psychiatry Units (MPUs) in Cultural Context: Lessons from MPUs in the Netherlands, the United States and Korea. [Conference presentation]. ICPM World Congress,Tuebingen, Germany.
Interested in conducting research within our Medicine in Psychiatry services?
Looking for more information and support on how best to work with our clinical staff to recruit patients receiving acute and primary medical care?
We will provide; consultation for clinical investigators interested in conducting research within our Medicine in Psychiatry (IMIP) services, including feedback about project proposals, consultation around the logistics related to launching research projects within our unique clinical settings, and assistance collaborating with our clinical teams.
Submit Research ProjectFaculty

Kirk Harris
Chief of Clinical Service

Marsha Wittink
Chief of Academic Affairs