Department News
Farewelcome to Medicine Trainees
Wednesday, June 25, 2025
June is a bittersweet time of year for medical trainees. It marks the end of one chapter—filled with long hours, complex cases, and indelible bonds with peers—and the beginning of the next.
Farewell
Throughout the past month, the DOM recognized and celebrated the achievements of our outgoing trainees—and held a friendly resident-faculty Jeopardy competition (complete with colorful and creative costumes).
Whether trainees are staying at URMC or continuing their careers on distant shores, DOM Chair Ruth O’Regan, MD, urges them to “hold the spirit of Meliora and always strive for better. Approach your roles with curiosity, humility, and a commitment to lifelong learning. Push boundaries, challenge norms, and seek to improve the lives of those you serve.”
Please join us in congratulating our graduating residents (pictured below) and fellows (see fellows slideshow).

2025 Internal Medicine Residency graduates Front: Keyan Zarei, MD, PhD, Jade Walden, MD, Nataliia Paone Aerton, MD, Aneliya San, MD, Anne Zhang, MD, Maya Shumyatcher, MD, Rachel Turner Hilley, MD, and Xingyi Shi, MD. Second row: Nina Rizk, MD, MPH, MS, Christina Moore, MD, Emma Hassell, MD, Lauren Lewis, MD, Louis Arens, MD, Michael Tiongson, MD, and Tony Sun, MD, PhD. Third row: Kelsey LaPiano, MD, Meghan DioGuardi, MD, Kristen Clements, MD, PhD, Anan Kazi, MD, and Casey Storms, MD. Fourth row: Rohith Palli, MD, PhD, Neesha Desai, MD, Joseph Glick, MD, and Jean Lafontant, MD, MPH. Top row: Seif Nasir, MD, MPH, Troy Anlage, MD, and Filip Koritysskiy, MD. Photo credit: Alliet Photography.

2025 Medicine-Pediatrics Residency graduates Front: Jennifer Tich, MD, Sonia Joshi, MD, Grace Ng, MD, and Kunali Gurditta, MD. Middle: Jenny Beuschel, MD, Rebekah Roll, MD, and Amanda Kaley, MD. Back: Justin Lansinger, MD, and Michelle Prong Geiger, MD. Photo credit: Alliet Photography.
Welcome
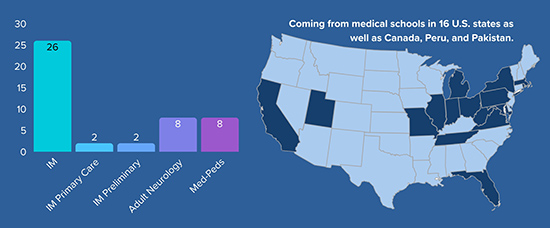
In June, we also welcomed a new crop of medical trainees. This year 46 new residents joined our ranks, 26 in Categorical Internal Medicine (IM), two in IM Primary Care, two in IM Preliminary, eight in Adult Neurology, and eight in Medicine-Pediatrics. The University of Rochester and University at Buffalo supplied the largest number of residents in this cohort, with seven residents each. Others came to us from medical schools in 16 U.S. states as well as Canada, Peru, and Pakistan.
Congratulations and welcome to our incoming residents! View a slideshow of incoming residents.
Aging Experts Share Wisdom at American Geriatrics Society Meeting
Tuesday, June 24, 2025
Geriatrics/Aging faculty members and fellows had a strong showing at the 2025 annual scientific meeting of the American Geriatrics Society (AGS) in Chicago in May.
As co-PI of the Geriatrics Workforce Enhancement Program (GWEP), Thomas Caprio, MD, of Geriatrics/Aging, moderated the GWEP pre-conference session.
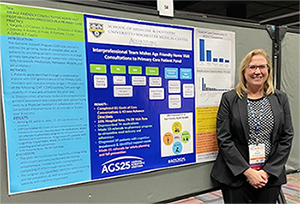
Lisa Vargish, MD, MS
Lisa Vargish, MD, MS, of Geriatrics/Aging, was elected by a national vote to serve as chair of the AGS Teacher’s Section. She also presented the poster “An Age-Friendly Consultative Home Visit Pilot Program Embedded in a Primary Care Practice” as part of the Presidential Poster Session.
Mary Bonnett, MD, of Geriatrics/Aging, led a Geriatric Academic Career Award Special Interest Group session.
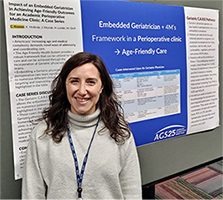
Courtney Kramer, MD
Courtney Kramer, MD, Geriatric Medicine fellow, presented the poster “Impact of an Embedded Geriatrician in Achieving Age-Friendly Outcomes for an Academic Perioperative Medicine Clinic.”
Sarah Morgan, MD, Geriatric Medicine fellow, presented the poster “Digging Deeper into Anxiety Symptoms: A Case of Serotonin Syndrome Related to Post-Strok Neurostimulant Use.”
Kah Poh (Melissa) Loh, BMedSci, MBBCh, BAO, MS, of Hematology/Oncology, presented the poster “Strategies to Advance Research through inclusive of Diverse older Adults and Artificial Intelligence in Aging Research and Clinical Care.”

Photo caption: (left to right) Heather Lander, MD,
Annie Medina-Walpole, MD, and Jennifer
Muniak having fun at the AGS Dance Party.
Laura Robinson, MPH, program coordinator of the Finger Lakes Geriatrics Education Center, presented “Promoting Age-Friendly Care & Career Development Across Specialties: The Geriatric-Faculty Scholars Program” as part of the Education Paper Session.
Additional co-authors include Jennifer Muniak, MD, Medicine, Highland Hospital; Katlyn McBride, MD, of Geriatrics/Aging; Suzanne Gillespie, MD, of Geriatrics/Aging; Annette Medina-Walpole, MD, of Geriatrics/Aging; Dallas Nelson, MD, of Geriatrics/Aging; Dana Stanton, PAC of Geriatrics/Aging; and Lauren O’Connor, PAC, of Internal Medicine.
Nephrology, Endocrinology Fellows Jump the Shark (Tank)
Tuesday, June 24, 2025

From back left: Marilyn Augustine, MD, Janany Sabescumar, MD, James Rutowski, MD
(Neph), Katherine Hazen, MD (Endo), Frantzcess Compas, MD (Endo), Hira Khan, MBBS
(Endo), and Hye Jeong Han, DO (Endo). Front from left: Scott Liebman, MD, MPH, Sara
McLeod, DOO, MPH, and Erica Miller, MD
Nephrology and Endocrinology fellows participated in a Shark Tank-style competition at the culmination of a year-long curriculum devoted to ensuring optimal health for all. Teams of fellows presented their projects developed over the course of the year and were judged by “Sharks” Sara Macleod, DO, MPH of Endocrine/Metabolism, Erica Miller, MD of Cardiology, and Scott Liebman, MD, MPH of Nephrology.
Four teams competed for bragging rights and Endocrinology fellows Katherine Hazen, MD and Fadila Noor, MBBS won the competition with their project, “Disparities in Diabetes Technology: A Study of Access and Outcomes Related to Continuous Glucose Monitoring.”
This was the first year Nephrology and Endocrinology teamed up for such a program and they hope to make it an annual occurrence, according to faculty champions Marilyn Augustine, MD of Endocrine/Metabolism, and Janany Sabescumar, MD of Nephrology.
Home is Where the Hospital Is: Hospital at Home Program Launching in September
Thursday, June 12, 2025
 Meet Edna, a fiercely independent 82-year-old who lives alone with family support. The last place Edna wants to be is in the hospital, but she can’t ignore her worsening shortness of breath and swelling legs.
Meet Edna, a fiercely independent 82-year-old who lives alone with family support. The last place Edna wants to be is in the hospital, but she can’t ignore her worsening shortness of breath and swelling legs.
Under the current UR Medicine system, Edna would be admitted to the hospital to receive acute care for heart failure for days or possibly weeks. But with a new Hospital at Home (HaH) program, launching this September, Edna will be able to get the inpatient care she needs in the comfort of her own home.
UR Medicine Hospital at Home combines advanced remote monitoring, telehealth technology, and in-home clinical visits to deliver hospital-level care in a more comfortable and personalized setting. The program reflects UR Medicine’s commitment to addressing ongoing hospital capacity challenges while working to improve patient satisfaction and outcomes.
Why This Matters
We anticipate the HaH program will enhance clinical team satisfaction and strengthen our connection to the patients we serve. Here’s how:
- Patient-Centered Care: Patients experience the therapeutic impact of receiving treatment and recovering in familiar surroundings, which promotes comfort and healing.
- Improved Outcomes: When HaH is compared to traditional inpatient hospitalization, studies have shown comparable or better clinical outcomes, reduced readmissions, and higher patient satisfaction scores.
- Community Impact: HaH can expand access to care for populations facing barriers to traditional hospital services.
- System Efficiency: By easing inpatient bed shortages, HaH supports our strategic goals for tertiary and quaternary care.
HaH is being developed under the leadership of Justin Hopkin, MD, chief of Hospital Medicine, Shayne Hawkins, RN, director of Med/Surg Nursing, and Kelly Luther, MSW, senior director of Social Work and Patient & Family Services. The program’s clinical and administrative leaders include Clare Park, DO, of Hospital Medicine (medical director), Heather Jackson, MS, RN, (senior nurse manager), and Michelle B. Maxon, MBA, (administrative director).
HaH will start with a small patient census and scale gradually to ensure quality oversight and seamless care delivery. Additional resources, including an intranet page and public-facing website, are coming soon.
To learn more about HaH, watch this month’s DOM Town Hall, featuring a presentation by program leader Justin Hopkin, MD.
Email HospitalAtHome@urmc.rochester.edu with any questions.
Celebrating Resident Excellence
Wednesday, June 11, 2025
Two Internal Medicine residents were honored for leading innovative research and quality improvement initiatives, earning the annual Resident Excellence Awards in Quality Improvement and Research Grand Rounds. Please join us in congratulating this year’s winners:
Quality Improvement
 Joseph Glick, MD
Joseph Glick, MD
Mentor: Catherine Glatz, MD, of Hospital Medicine
Mitigating Excessive Laboratory Testing in Hospitalized Patients: An Interdisciplinary Quality Improvement Initiative
Excessive laboratory testing can be harmful, costly, and futile to patients. Since 2022, Joseph Glick, MD, along with an interdisciplinary team, has implemented a quality improvement project to decrease excessive lab testing across the 6-1400 and 6-3400 units. Glick’s team implemented educational interventions for physicians and nurses that reduced the median number of lab tests per patient encounter by 18%, but the reduction was not sustained. Subsequent surveys showed a majority of physicians and nurses support reducing labs and feel that more fully utilizing the EMR (for example, to place limits on the duration of lab orders, and flags prompting lab reduction for medically ready or ALC patients) may help promote a sustained decrease. The team is now planning to implement structured education for first- and second-year resident orientations and taking a closer look at developing an EMR integration.
Research
 Aneliya San, MD
Aneliya San, MD
Mentor: Mehmet Aktas, MD, of Cardiology
Sex Hormone-Dependent Modulation of Cardiac Repolarization During the Menstrual Cycle in Women Treated with QT-Prolonging Drugs
Many medications, including antiarrhythmics, antibiotics, and antipsychotics, can disrupt normal heart rhythms by prolonging the QT interval and women are disproportionately impacted by drug-induced QT prolongation. Aneliya San, MD, examined how hormonal fluctuations throughout the menstrual cycle affects drug-induced QT prolongation. San mapped ECG recordings to hormone levels in 41 women: 20 treated with drugs known to prolong the QT interval and 21 controls. Results confirmed a drug-hormone interaction, with increased estrogen exacerbating drug-induced QT prolongation and higher progesterone-estradiol ratios correlating with shorter QT intervals. The takeaway: women of reproductive age should be closely monitored when prescribing QT-prolonging drugs, and treatment should be tailored based on hormonal influences.
Watch a recording of the grand rounds to learn more about awardees’ projects.
GI Team Gets Gutsy at Digestive Disease Week
Wednesday, June 11, 2025
 “Be Gutsy” was the theme of this year’s Digestive Disease Week, the premier meeting of digestive health clinicians, researchers, and industry professionals from around the world. Eight members of our Gastroenterology & Hepatology Division were among 13,000 attendees, and delivered 12 presentations, 12 posters, and two original lectures, and moderated two sessions.
“Be Gutsy” was the theme of this year’s Digestive Disease Week, the premier meeting of digestive health clinicians, researchers, and industry professionals from around the world. Eight members of our Gastroenterology & Hepatology Division were among 13,000 attendees, and delivered 12 presentations, 12 posters, and two original lectures, and moderated two sessions.
Sarah Enslin, PA-C, physician assistant of Gastroenterology & Hepatology, presented, “Incorporating APPS into Your Endoscopic Practice to Promote Improved Patient Satisfaction.” She also participated in an AGA-sponsored panel discussion, “Career Planning for GI NPs and Pas.”
Vivek Kaul, MD, professor of Gastroenterology & Hepatology, presented the Distinguished Abstracts Plenary Session of the AGA presentation ceremony and delivered five presentations and four posters:
- Mentorship in Advanced Endoscopy (Presentation)
- Are You Smarter Than Your Mentor: Management of Pancreatic Cystic Neoplasms (Presentation)
- Novel Technologies for Screening, Surveillance and Treatment of Barrett's Esophagus (Presentation)
- Progression Rates of Barrett's Esophagus and Dysplasia Detected by WATS-3D are Similar to Those Diagnosed by Forceps Biopsies (Presentation)
- Late Breaking Clinical Abstracts Plenary (Presentation)
- Blood-based Testing Practices Amongst High-risk Individuals Undergoing Pancreatic Cancer Surveillance within the International Pancreatic Cancer Early Detection (PRECEDE) Consortium (Poster)
- Consensus Recommendations for Liquid Nitrogen Spray Cryotherapy for BE Using a Modified Delphi Process (Poster)
- Consensus Recommendations for Liquid Nitrogen Spray Cryotherapy for Esophageal Cancer Using a Modified Delphi Process (Poster)
- MUC2 Immunostaining Predicts Neoplastic Progression as Accurately as the Presence of Goblet Cells in ColumnarLined Esophagus: A Wats3D Study of 3553 Patients (Poster)
- Controversial Areas in Pancreatic Cancer Surveillance: A Survey Across the International Pancreatic Cancer Early Detection (PRECEDE) Consortium (Poster)
 Shivangi Kothari, MD, assistant professor of Gastroenterology & Hepatology, presented “Optimal Strategies for Colonic Polyp Management: When to choose EMR or ESD,” and moderated the session “Training, Technology, and Tackling Challenges in Clinical Practice.”
Shivangi Kothari, MD, assistant professor of Gastroenterology & Hepatology, presented “Optimal Strategies for Colonic Polyp Management: When to choose EMR or ESD,” and moderated the session “Training, Technology, and Tackling Challenges in Clinical Practice.”
Truptesh Kothari, MD, MS, associate professor of Gastroenterology & Hepatology, presented two original lectures, “Role of EUS in Therapeutic Oncology” and “Kothari EUS-FNA Techniques,” and moderated “A New Frontier in Gastrointestinal Endoscopy: The Cutting-Edge Developments in Gastrointestinal Endoscopy.” He also delivered two presentations and four posters:
- Endoscopic Ultrasound (Presentation)
- DDW Clinical Science Late-Breaking Abstract Plenary (Presentation)
- Training, Technology, and Tackling Challenges in Clinical Practice (Poster)
- Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD) and Metabolic Dysfunction-Associated Steatohepatitis (MASH) (Poster)
- Cholelithiasis and Biliary Tract Disorders (Poster)
- Endoscopic Retrograde Cholangiopancreatography (ERCP) (Poster)
Danielle Marino, MD, associate professor of Gastroenterology & Hepatology, delivered the presentation “Medical Education Face-Off: Debating Hot Button Issues of GI Training,” and the poster “BarberED, BeautiED, Then Screened (BBTS).”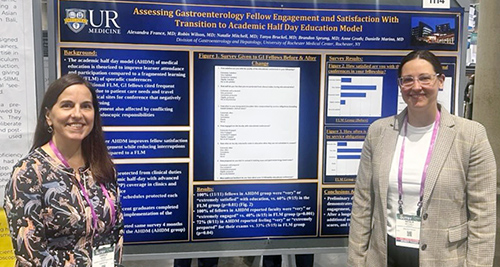
Natalie Mitchell, MD, Gastroenterology fellow, presented the poster “Assessing Gastroenterology Fellow Engagement and Satisfaction with transition to academic half day education model.”
Patrick Twohig, MD, MPH, assistant professor of Gastroenterology & Hepatology, co-presented the posters, “Comparative Risks of GERD, Gastric Intestinal Metaplasia, and Upper GI Cancers in Obesity Patients: A Propensity-Matched Population-Based Study of Bariatric Surgery vs GLP-1 Receptor Agonists” and “HCC and Mortality Risk Across Cirrhosis Etiologies: A Nationwide Population-Based Study” alongside mentee Emily Shu-Yen Chan, MD, MS.
2025 Pilot Awardees Will Tackle Everything from Microplastics to Contraception
Thursday, May 22, 2025
The Department of Medicine funds promising research, quality, and educational initiatives through its Research and Education Pilot Awards program. Awardees receive $20,000-$40,000 for basic, clinical, or translational research or educational scholarship projects.
Congratulations to this year’s awardees, who will kick their projects off on July 1:
Optimizing cardiac imaging in women with early-stage breast cancer
 Approximately 20% of breast cancers overexpress human epidermal growth factor 2 (HER2). While HER2-targeted therapies improve survival, they also increase the risk of heart failure. Current guidelines recommend that all women receive cardiac imaging every three months during treatment, regardless of their risk of cardiotoxicity. Farhan Bajwa, MD, assistant professor of Cardiology, will study whether tailoring the frequency of cardiac imaging to each patient’s baseline risk of cardiotoxicity (prior to cancer treatment) reduces harm and waste.
Approximately 20% of breast cancers overexpress human epidermal growth factor 2 (HER2). While HER2-targeted therapies improve survival, they also increase the risk of heart failure. Current guidelines recommend that all women receive cardiac imaging every three months during treatment, regardless of their risk of cardiotoxicity. Farhan Bajwa, MD, assistant professor of Cardiology, will study whether tailoring the frequency of cardiac imaging to each patient’s baseline risk of cardiotoxicity (prior to cancer treatment) reduces harm and waste.
Evaluating curriculum for hospitalists and residents in caring for patients with an eating disorder
 Adults who receive adequate care can recover from eating disorders, yet eating disorders have the second-highest mortality rate of all mental health disorders due to a lack of access to care. Adam Bracken, MD, assistant professor of Hospital Medicine and Pediatrics, will develop and evaluate a curriculum to train Hospital Medicine faculty and APPs, and Internal Medicine residents to diagnose and manage patients with eating disorders. The curriculum for faculty and APPs would include three one-hour sessions with an opportunity for a simulated patient experience. The resident curriculum is a two-week elective with rotations on inpatient units. Both curricula will be assessed iteratively using the Context, Input, Process, and Product evaluation model.
Adults who receive adequate care can recover from eating disorders, yet eating disorders have the second-highest mortality rate of all mental health disorders due to a lack of access to care. Adam Bracken, MD, assistant professor of Hospital Medicine and Pediatrics, will develop and evaluate a curriculum to train Hospital Medicine faculty and APPs, and Internal Medicine residents to diagnose and manage patients with eating disorders. The curriculum for faculty and APPs would include three one-hour sessions with an opportunity for a simulated patient experience. The resident curriculum is a two-week elective with rotations on inpatient units. Both curricula will be assessed iteratively using the Context, Input, Process, and Product evaluation model.
Using AI to improve clinicians’ communication with older patients with advanced cancer
 Ehsan Hoque, MD, professor of Computer Science, will develop and test the AI platform, SOPHIE, to help clinicians improve communication skills for serious illness conversations with advanced cancer patients. SOPHIE allows clinicians to practice conversations with a virtual patient and receive real-time feedback to improve clarity, empathy, and patient empowerment. Hoque and Epstein will create scenarios reflecting diverse clinical situations to enhance communication, particularly with underserved and low-literacy populations.
Ehsan Hoque, MD, professor of Computer Science, will develop and test the AI platform, SOPHIE, to help clinicians improve communication skills for serious illness conversations with advanced cancer patients. SOPHIE allows clinicians to practice conversations with a virtual patient and receive real-time feedback to improve clarity, empathy, and patient empowerment. Hoque and Epstein will create scenarios reflecting diverse clinical situations to enhance communication, particularly with underserved and low-literacy populations.
Characterizing the infusion of microplastics to patients undergoing cardiopulmonary bypass
 Cardiopulmonary bypass pumps, which are used in over 90% of cardiac surgeries, have many flexible and compressible components made of the synthetic polymer, polyvinyl chloride (PVC).
Cardiopulmonary bypass pumps, which are used in over 90% of cardiac surgeries, have many flexible and compressible components made of the synthetic polymer, polyvinyl chloride (PVC).
Mark Marinescu, MD, assistant professor of Clinical Medicine, Cardiology, will investigate if PVC or other synthetic polymers leach into patient blood during bypass support in the form of microplastics. Preliminary findings indicate that contamination from the cardiopulmonary bypass circuit is introduced into the priming solution despite using a pre-bypass filter. How these microplastics impact health is still unknown.
Comparing six-minute walk test to cardiopulmonary exercise test
 Nearly half of patients hospitalized with acute pulmonary embolism report breathlessness and functional limitation three months later. These patients often undergo cardiopulmonary exercise testing (CPET) to evaluate physiologic abnormalities during exercise, but this test does not replicate patients’ normal weight-bearing activities and is too strenuous to administer within three months of an acute pulmonary embolism. Dominick Roto, DO, assistant professor of Pulmonary Diseases and Critical Care, will investigate whether a six-minute walk test with incorporated CPET measurements can produce similar testing results as the traditional maximal-effort CPET. The six-minute walk test does not require strenuous exercise or expensive equipment and better replicates patients’ normal activity, suggesting it may be a safe and cost-effective alternative for early functional assessment of post-pulmonary embolism impairment.
Nearly half of patients hospitalized with acute pulmonary embolism report breathlessness and functional limitation three months later. These patients often undergo cardiopulmonary exercise testing (CPET) to evaluate physiologic abnormalities during exercise, but this test does not replicate patients’ normal weight-bearing activities and is too strenuous to administer within three months of an acute pulmonary embolism. Dominick Roto, DO, assistant professor of Pulmonary Diseases and Critical Care, will investigate whether a six-minute walk test with incorporated CPET measurements can produce similar testing results as the traditional maximal-effort CPET. The six-minute walk test does not require strenuous exercise or expensive equipment and better replicates patients’ normal activity, suggesting it may be a safe and cost-effective alternative for early functional assessment of post-pulmonary embolism impairment.
Impact of weight gain perceptions on hormonal contraceptive selection
 Hormonal contraceptives are highly effective, but women with overweight or obesity may be more likely to discontinue them due to weight gain concerns. Adnin Zaman, MD, assistant professor of Endocrine/Metabolism, will develop and validate a novel, patient-centered survey to assess women’s experience and perceptions of weight-related side effects of hormonal contraceptives. In the long term, this survey could serve as a clinical tool to help providers tailor contraceptive counseling.
Hormonal contraceptives are highly effective, but women with overweight or obesity may be more likely to discontinue them due to weight gain concerns. Adnin Zaman, MD, assistant professor of Endocrine/Metabolism, will develop and validate a novel, patient-centered survey to assess women’s experience and perceptions of weight-related side effects of hormonal contraceptives. In the long term, this survey could serve as a clinical tool to help providers tailor contraceptive counseling.
DOM Faculty and Trainees Showcase Collaborative Work at SGIM Annual Meeting
Wednesday, May 21, 2025
Faculty and trainees representing Primary Care, General Medicine, Hospital Medicine, and the Medicine-Pediatrics Residency showcased their cross-departmental collaborative work at the Society of General Internal Medicine annual meeting. This year’s meeting held May 14-17 in Hollywood, FL, focused on how academic general internists are changing the healthcare landscape.

DOM faculty and trainees presented on a range of education and research projects:
Robert Fortuna, MD, MPH, professor of Internal Medicine and Primary Care, presented “Medical Resident Clinic Directors: Faculty Roles, Scheduling, Coverage Strategies, and Inclusion of Advanced Practice Partners.”
Kunali Gurditta, MD, Medicine-Pediatrics Resident, and M. Mahala Schlagman, MD, assistant professor of General Medicine, presented the poster “Implementing an Accessibility Activity to Improve Education on Ableism for Internal Medicine Residents.” Other DOM coauthors include Amy Blatt, MD, director of the Internal Medicine Residency. Gurditta started this work in the Hoekelman Center as part of the Community Health & Advocacy Resident Education track.
Sara Gianfagna, DO, MSMEd, assistant professor of General Medicine, presented the poster “Nursing, Pharmacy and Nutrition: oh my! Teaching to Improve Utilization of our Interdisciplinary Team for Diabetes Education During Ambulatory Education Sessions.” Other DOM coauthors include Catherine Gracey, MD, DOM vice chair for education and interim chief of General Medicine.
Jennifer Joy Beuschel, MD, Medicine-Pediatrics Resident, presented the poster “Intersection of Social Vulnerability, Social Drivers, Race and Hypertension.” Other DOM coauthors include Rebekah Roll, MD, Medicine/Pediatrics resident, John S. Clark, MPP, chief administrative office for Primary Care, and Robert Fortuna, MD, MPH.
David Staudt, MD, assistant professor of Hospital Medicine, presented the poster "Ripple Effects: The Impact of Preclinical Ultrasound "Homework" on Medical Student Attitudes and Behaviors" and the workshop "Practical POCUS: How to safely integrate trainee-driven POCUS into medical decision-making with minimal ultrasound training"
Jennifer Pascoe, MD, associate professor of Hospital Medicine, also attended.
Caprio to Serve as Acting Chief of Geriatrics During Medina-Walpole Sabbatical
Thursday, May 15, 2025

Thomas Caprio, M.D.

Annette Medina-Walpole, M.D.
Annette Medina-Walpole, MD, will temporarily step down as chief of the Division of Geriatrics/Aging to focus on her role as director of the UR Aging Institute (URAI). Academic geriatrician Thomas Caprio, MD, will serve as acting division chief during Medina-Walpole’s year-long sabbatical, starting July 1.
“Tom’s training and expertise span the clinical, research, and education missions, and he has proven himself as both an institutional and national leader in geriatrics,” said Department of Medicine Chair Ruth O'Regan, MD. “His experience and expertise make him a great fit for this position, and I look forward to working with him over the next year.”
Caprio is a geriatrician and hospice/palliative care physician, serving as chief medical officer of UR Medicine Home Care, medical director of UR Medicine Hospice, and professor of Geriatrics, Dentistry, Psychiatry, Public Health Sciences, and Clinical Nursing. He also directs the Finger Lakes Geriatric Education Center.
Caprio leads research that improves care delivery for older adults. He studies how interdisciplinary approaches, such as geriatrics-related educational programs for health care professionals, can improve care and outcomes for aging patients with complex needs. He also investigates ways to improve health care policies affecting home care, hospice services, and long-term care.
As acting chief, Caprio will oversee the division’s education, research, and clinical care programs and over 45 faculty members who provide care for thousands of older adults each year. He will maintain the division’s role in shaping the future of healthcare delivery to older adults in the region.
“I am deeply honored to take on this role and continue to support the University of Rochester’s national reputation for excellence in geriatrics," said Caprio. “I’m excited to continue building our collaborative clinical teams as we provide age-friendly care throughout our health system and advocacy for funding to support our ongoing work in research and education.”
Over the next year, Medina-Walpole will develop a five-year strategic plan for the URAI that aligns with UR Boundless Possibilities and URMC strategic plans.
The URAI integrates aging-related expertise in research, patient care, education, and community outreach across the University to empower older adults to age with vitality. Since its inception in 2019, the institute has helped researchers procure over $40 million in new funding, developed strong collaborations across the University and community organizations, established a training grant in Alzheimer’s Disease, and led URMC’s Age-Friendly Health Care System transformation.
“The UR Aging Institute has had an incredibly successful start,” said Medina-Walpole. “Now, it’s time to bring the institute to the next level, in line with other premier national aging institutes. My academic leave will focus on establishing future directions and priorities that build on our mission.”
Medina-Walpole will visit renowned aging programs at other prominent academic institutions to draw inspiration from their operational models. She will also conduct a listening tour across the University to identify new opportunities for collaboration across the URAI. A strategic planning taskforce and an external advisory board will help develop and evaluate the new URAI strategic plan.
Medina-Walpole plans to resume her role as Geriatrics/Aging chief and clinical duties on July 1, 2026.
Researchers Have Their Fingers on the Pulse of the Annual Heart Rhythm Society Meeting
Wednesday, May 14, 2025
Left to right: Valentina Kutyifa, MD, PhD, Ilan Goldenberg, MD, David Huang, MD,
Wojciech Zareba, MD, PhD, Claudio Schuger, MD, (of Wayne State University)
and Mehmet Aktas, MBA, MD
Cardiology researchers were among the more than 10,000 heart rhythm clinicians, allied professionals, scientists, and researchers who attended the Heart Rhythm Society’s annual meeting this year.
The meeting featured 200 educational sessions led by more than 2,000 experts, including:
Mehmet Aktas, MBA, MD, of Cardiology, presented a poster showing that the cancer drug, acalabrutinib, is associated with increased risk of atrial fibrillation in patients with lymphoproliferative disorders on behalf of lead author Saadia Sherazi, MBBS, MS, of Highland Hospital Medicine.
Ilan Goldenberg, MD, of Cardiology Heart Research, participated in a faculty debate arguing for the need to use risk stratification strategies prior to implanting a primary prevention implantable cardioverter device (ICD) in patients with ischemic or nonischemic heart failure.
Daniel Han, a student in the Medical Scientist Training Program, presented the poster “Non-Obese Patients with Metabolic Syndrome and Heart Failure Outcomes in ICD or Cardiac Resynchronization Therapy with Defibrillator (CRT-D) Patients in MEGA-MADIT,” a project that was mentored by Valentina Kutyifa, MD, PhD.
David Huang, MD, of Cardiology, presented the poster “Effects of Left Ventricular Assist Device (LVAD) Support on Recurrent Ventricular Arrythmias and ICD Therapies Among Advanced Heart Failure Patients: Comparing the PIVATAL and RAID Trials.”
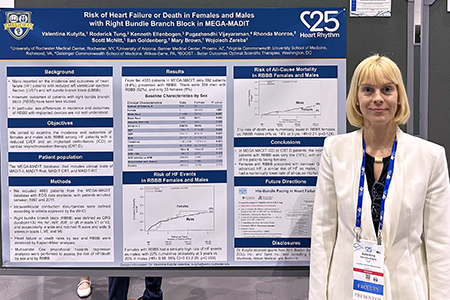 Valentina Kutyifa, MD, PhD, of Cardiology Heart Research, was part of a panel discussion on breaking down gender disparities in cardiovascular clinical trials leadership and hosted a research roundtable in the Fellows-in-Training Meet-the-Mentors session. She also had a late-breaking oral presentation, “Contemporary Outcomes of Non-Ischemic Cardiomyopathy Patients with Implanted Devices” related to BIO-LIBRA, a multicenter clinical study on non-ischemic cardiomyopathy, led by the University of Rochester in collaboration with Biotronik. Kutyifa also presented a poster “Risk of Heart Failure or Death in Men and Women with RBBB in MEGA-MADIT,” to provide information on outcomes of this cohort.
Valentina Kutyifa, MD, PhD, of Cardiology Heart Research, was part of a panel discussion on breaking down gender disparities in cardiovascular clinical trials leadership and hosted a research roundtable in the Fellows-in-Training Meet-the-Mentors session. She also had a late-breaking oral presentation, “Contemporary Outcomes of Non-Ischemic Cardiomyopathy Patients with Implanted Devices” related to BIO-LIBRA, a multicenter clinical study on non-ischemic cardiomyopathy, led by the University of Rochester in collaboration with Biotronik. Kutyifa also presented a poster “Risk of Heart Failure or Death in Men and Women with RBBB in MEGA-MADIT,” to provide information on outcomes of this cohort.
Alexei Nakonechnyi, PhD, and Dillon Dzikowicz, PhD, RN, PCCN, of Cardiology Heart Research, presented two posters, “Dynamic Risk Stratification for Progression to Persistent Atrial Fibrillation in Patients with Cardiac Implanted Electronic Devices,” and “Machine Learning for Predicting Progression to Persistent Atrial Fibrillation Using Point-in-Time Risk Stratification.”
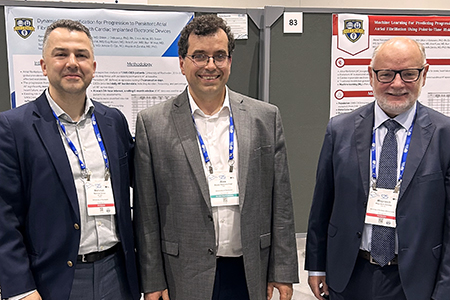
Amole Ojo, MD, of Cardiology, presented the poster “Risk Factors and Outcomes Associated with Failed Implantable Cardioverter Defibrillator Shocks,” and hosted an oral abstract session exploring the role and outcomes of cardiac resynchronization therapy (CRT) and conduction system pacing among patients in common, specific scenarios. He also participated as a mentor in the Fellows-in-Training and the Medical Student, Intern, & Resident Meet-the-Mentors Roundtables. Ojo also co-hosted the HRS Board Review Course, a refresher on electrophysiology fundamentals for physicians and fellows preparing for certification or recertification.
Wojciech Zareba, MD, PhD, of Cardiology and Cardiology Heart Research, presented two posters, “Clinical Phenotype of Variants of Uncertain Significance in Long QT Syndrome Patients by Genotype,” and “Clinical, Electrocardiographic, and Cardiac Magnetic Resonance Imaging Risk Factors Associated with Ventricular Tachyarrhythmias in Nonischemic Cardiomyopathy (MARVEN Study).”
MDS Foundation Honors Bennett with a Lifetime Achievement Award
Wednesday, May 14, 2025

John M. Bennett, MD
John M Bennett, MD, professor emeritus of Medicine, Hematology/Oncology and Pathology and Laboratory Medicine, and a founding leader of the now Wilmot Cancer Center, received a Lifetime Achievement Award from the Myelodysplastic Syndromes Foundation on May 8 at the 18th annual International Congress held in Rotterdam, the Netherlands.
Recognized for his leadership and pivotal contributions to the field, Bennett was the editor-in-chief of the Leukemia Research Journal for 20 years and served as the first chair of the Myelodysplastic Syndromes Foundation from 1997 to 2010.
He came to University of Rochester in July 1969, practicing a few years at Highland Hospital as head of the Hematology/Oncology program before shifting to Strong Memorial Hospital, which was in the beginning stages of forming a cancer center. Surgical Oncology, Radiation Oncology, and other departments came together to create the University of Rochester Cancer Center in 1974.
Bennett served as URCC clinical director from its inception until 1996, when he shifted to a part-time role with hematopathology. In those early years, he helped create the foundation for the center’s strength in attending to patients' psychosocial needs, commitment to educational programs, and national leadership in clinical trials that would help make today's cancer treatments possible.
A role model and dedicated mentor, many young physicians were drawn to Rochester to study with Bennett. He is a member of numerous professional societies and contributed more than 600 publications to medical literature as well as several books.
Reporting for Duty: Morning Report Room is Back in Use
Tuesday, May 13, 2025

After being sidelined for several months for renovations, the Morning Report room (7.2346/7.2366) returned to action on May 1. The beautifully renovated space features new technology and a sound system to support interactive, hybrid meetings, movable tables and chairs that allow room reconfiguration, six clinical workstations for residents and learners, and a kitchenette for our peckish physicians.
Residents and rotating medical students have swipe access to the space, which is typically used for Morning Report, noon conferences, residency meetings, patient handoffs, small team teaching, and patient care discussions. Trainees are welcome to use the workstations and kitchenette whenever the room is not in use for meetings.
DOM Heart Research on Display at EHRA 2025 in Vienna
Wednesday, April 30, 2025
DOM cardiac researchers traveled to Vienna, Austria at the end of March to present their work at the annual congress of the European Heart Rhythm Association (EHRA), part of the European Society of Cardiology.



Ilan Goldenberg, MD, of Cardiology Heart Research, hosted a steering committee meeting for the PRIMARY PREVENT VT trial, which is led by a team at the University of Rochester and included 20 centers in Europe. This innovative clinical trial is designed to evaluate novel ablation modalities to reduce the risk of arrhythmias and sudden death in patients with heart failure.
David Huang, MD, of Cardiology, delivered a Late Breaker Trial presentation on the rationale and design of PIVATAL, an NIH sponsored, multi-center trial investigating the role of intraoperative ventricular ablation in high-risk heart failure patients eligible for left ventricular assist devices. He also presented preliminary, blinded arrhythmia and clinical outcomes data from the patients enrolled thus far.
Valentina Kutyifa, MD, PhD, of Cardiology Heart Research, spoke in two sessions on implantable cardioverter defibrillator therapy and chaired a session on cardiac pacing. She attended a meeting as a member of the steering committee of the PROFID EHRA trial, which is investigating the role of the defibrillator with contemporary medical therapy in over 100 sites in Europe. Kutyifa also joined the EP Europace editorial board as associate editor of innovative technologies.
Strategic Plan: Expanding Robust Research to Achieve Breakthrough Discoveries
Wednesday, April 16, 2025
This is part of a series highlighting the Department of Medicine 2024-2028 Strategy and Action Plan, its five pillars for success, and progress toward meeting the goals.
Collaborative research that advances discovery is essential for success, and the DOM is committed to securing new funding to support further exploration.
To attain this goal, outlined in the Strategic Plan, the priorities are:
- Expand basic, translational, clinical, medical education, and DEI research through interdisciplinary teams across diverse disciplines;
- Increase accruals in clinical trials and expand clinical research across the lifespan of diverse populations; and,
- Enhance our national and international reputation via interdisciplinary research and collaboration.
 Laura Calvi, MDLaura Calvi, MD
Laura Calvi, MDLaura Calvi, MD Valentina Kutyifa, MD, PhDValentina Kutyifa, MD, PhD“We are focused on providing internal teams the tools and resources to prepare, submit and attain new grant awards,” said Valentina Kutyifa, MD, PhD, vice chair for Clinical Research. “New grants will lead to more groundbreaking scientific discoveries that improve patient care.”
Valentina Kutyifa, MD, PhDValentina Kutyifa, MD, PhD“We are focused on providing internal teams the tools and resources to prepare, submit and attain new grant awards,” said Valentina Kutyifa, MD, PhD, vice chair for Clinical Research. “New grants will lead to more groundbreaking scientific discoveries that improve patient care.”
Efforts to expand research through interdisciplinary teams are already yielding results:
- New grant awards: In fiscal year 2024, DOM was awarded $41.3 million in grants, with $7.6 million in new awards. Researchers from all divisions submitted 187 proposals and 67 projects were awarded. There are 488 active externally sponsored projects, 294 of which are clinical trials.
- Biostatistical Shared Resource: Launched in 2022, this program supports mentored faculty and trainee researchers who do not have funding to cover their activities. Areas of support include study preparation and pre-study planning, sample size, basic statistics, multivariate regression, non-parametric tests, correlations, basic survival analyses and database management. Laura M. Calvi, MD, vice chair for Basic and Translational Science, is spearheading the biostatistical shared resource program.
- Division faculty research delegates: Delegates representing each division’s basic and clinical research identify areas of improvement, and design and launch new initiatives to expand current research efforts.
- New research website: launched in 2024, provides a centralized platform for showcasing research, publications, collaborations, research teams, and resources. It is designed to be a resource for internal team members, external collaborators and the broader community. The research leadership team is supported by Stefanie Fingler, MBA, director of Research Operations, and Kari Steinmetz, assistant director of Clinical Research.
Activities also are underway to increase clinical trial accruals:
- Initial study feasibility process: In January, leaders unveiled a new standard operating procedure for feasibility of clinical trials as part of a new, comprehensive clinical trials platform. Its primary mission is to achieve translation through clinical trials, with the goal of creating a uniform framework to identify innovative studies that align with the missions of DOM’s various divisions.
- OnCore use policy: To harmonize OnCore use across the department, active studies must be entered into the clinical trial management system. This allows for accurate tracking of study status, subject recruitment, and patient demographics.
- Ongoing study feasibility process: A pilot initiative is in place to assess ongoing study feasibility. All DOM clinical research protocols will be reviewed semi-annually and annually to ensure adequate scientific progress.
Another priority is to expand collaborations and research abroad. New initiatives in this area include the Uganda Program, led by Paul R. Bohjanen, MD, PhD, chief of Infectious Diseases, with the aim to develop a Global Health Program focusing on infectious diseases research and treatment. And, a program aimed at initiating new scientific and educational programs with the National University of Sciences & Technology in Islamabad, Pakistan is being led by Bilal Ahmed, MD, FACP, FRCP, of Internal Medicine.
National Champs: Wilmot Future Deaf Scientists Program Recognized at Deaf Education Conference
Tuesday, April 15, 2025
DOM Chair Ruth O’Regan, MD, and fellow co-director of the Wilmot Future Deaf Scientists Program, Wyatte Hall, PhD, received the National Champion Award from the Conference of Educational Administrators of Schools and Programs for the Deaf (CEASD) last week. O’Regan and Hall were honored for their “visionary leadership in establishing and expanding the [Wilmot] Future Deaf Scientists program,” which introduces deaf and hard-of-hearing high school students to the world of science and medicine with a focus on cancer research.
The National Champion Award honors stakeholders external to the CEASD for, “exemplary strategic assistance, substantive financial or programmatic support, legislative or policy advocacy, or other unique efforts which directly impact the success of CEASD on behalf of the member schools and programs, students and their families.”
 Hall (right) and McLetchie (left) accepted the award at the CEASD meeting in Pittsburgh on behalf of O’Regan and the entire Wilmot Future Deaf Scientists team.The Wilmot Future Deaf Scientists Program began as a partnership between the Wilmot Cancer Institute and the Rochester School for the Deaf in 2021, offering a four-week summer internship at Wilmot for RSD high school students. Last summer, the program secured funding from the National Cancer Institute to expand its programming to four other cancer centers who will collaborate with their respective local schools for the Deaf. This summer, the internship will be offered for the first time at Yale Cancer Center, Stanford Cancer Institute, Indiana University Simon Comprehensive Cancer Center, and University of Kentucky Markey Cancer Center.
Hall (right) and McLetchie (left) accepted the award at the CEASD meeting in Pittsburgh on behalf of O’Regan and the entire Wilmot Future Deaf Scientists team.The Wilmot Future Deaf Scientists Program began as a partnership between the Wilmot Cancer Institute and the Rochester School for the Deaf in 2021, offering a four-week summer internship at Wilmot for RSD high school students. Last summer, the program secured funding from the National Cancer Institute to expand its programming to four other cancer centers who will collaborate with their respective local schools for the Deaf. This summer, the internship will be offered for the first time at Yale Cancer Center, Stanford Cancer Institute, Indiana University Simon Comprehensive Cancer Center, and University of Kentucky Markey Cancer Center.
This fall, the program will also implement a new year-round curriculum for RSD students. Wilmot researchers and medical professionals will deliver classroom lessons and fireside chats at RSD throughout the school year culminating in an expanded summer internship at Wilmot.
“Students have expressed life-changing impacts, with some identifying career goals in nursing and medicine as a direct result of their participation,” said RSD Superintendent and CEASD board member Anthony McLetchie in a letter nominating O’Regan and Hall for the award. “Drs. Hall and O'Regan have created not just an academic initiative but a transformative model for fostering scientific ambition, representation, and equity among Deaf youth. Their dedication to removing systemic barriers and empowering Deaf students exemplifies the spirit of the National Champion Award, and we are immensely proud to celebrate their far-reaching contributions to our school and the broader Deaf community.”
Teaching Together After All these Years: DOM Faculty Meet at Internal Medicine Conference
Tuesday, April 15, 2025
 (Left to right) Catherine Tan, MD, Eric Anish, MD, and Diego Cahn-Hidalgo, MD, pose at the ACP Internal Medicine meetingNearly thirty years after serving as chief residents together in the DOM’s Internal Medicine Residency Program, Catherine Tan, MD, Diego Cahn-Hidalgo, MD, members of our Primary Care, and Eric Anish, MD, now an internist at the University of Pittsburgh Medical Center, taught together once again at the American College of Physicians (ACP) Internal Medicine Meeting in early April.
(Left to right) Catherine Tan, MD, Eric Anish, MD, and Diego Cahn-Hidalgo, MD, pose at the ACP Internal Medicine meetingNearly thirty years after serving as chief residents together in the DOM’s Internal Medicine Residency Program, Catherine Tan, MD, Diego Cahn-Hidalgo, MD, members of our Primary Care, and Eric Anish, MD, now an internist at the University of Pittsburgh Medical Center, taught together once again at the American College of Physicians (ACP) Internal Medicine Meeting in early April.
The trio, who had kept in touch but hadn’t taught together since their 1997-98 chief residency days, held a workshop to teach internal medicine and primary care physicians and trainees how to perform joint injections.
“Primary care physicians don’t perform a lot of procedures. We wanted to build their confidence to give these injections, so they don’t have to refer patients to an orthopedist,” said Tan. “We can save patients a lot of time and pain this way, not having to wait for another appointment.”
The trio’s arthrocentesis and bursal injection workshop was one of over 200 sessions at the ACP meeting offering professional development and best practices in patient care. The ACP is the largest medical specialty organization in the U.S. and Tan describes its annual meeting as the “Superbowl of Internal Medicine.”
The meeting brings together Internal Medicine physicians, trainees, and allied health professionals from all corners of the globe and all walks of life.
Tan and Cahn-Hidalgo were not the only DOM members to attend this year’s event in New Orleans. The following also represented DOM:
- Leslie Algase, MD, FACP, of Primary Care, who is on the board of regents for the ACP, helped host a UR Internal Medicine Residency reception and mentored during the Women in Medicine Networking Luncheon sponsored by ACP.
- Edward Chin, MD, who completed an Internal Medicine residency at URMC and is now an endocrinologist at the Medical College of Georgia, received Mastership at this year’s meeting. Mastership is an award honoring “highly accomplished persons demonstrating impact in practice, leadership, or in medical research.”
- Lisa C. Schwartz, MD, of Primary Care was inducted as a new ACP fellow, a peer-reviewed and supported credential that reflects excellence in internal medicine.
- Valerie Newman, MD, of Primary Care, who is the Rochester district president of NYACP, and Meghan DioGuardi, MD, an Internal Medicine Resident, also attended.
Strategic Plan: Supporting a Thriving Workforce and Culture
Wednesday, April 2, 2025
This is part of a series highlighting the Department of Medicine 2024-2028 Strategy and Action Plan, its five pillars for success, and progress toward meeting the goals.
 The DOM prioritizes wellness and education for faculty, staff and learners, because engaged and healthy workforce supports quality patient care. The Strategic Plan outlines its mission of cultivating a thriving workforce and culture.
The DOM prioritizes wellness and education for faculty, staff and learners, because engaged and healthy workforce supports quality patient care. The Strategic Plan outlines its mission of cultivating a thriving workforce and culture.
“Delivering outstanding, compassionate care to patients and achieving an engaged, healthy workforce are not mutually exclusive,” said Allen P. Anandarajah, MBBS, associate chair for Wellness.
“We want to provide the support our team needs to attain their goals and cultivate a workforce that is proudly striving to achieve the missions of the DOM and the Medical Center.”
The focus is to:
- Support and promote faculty and staff well-being;
- Provide professional development opportunities for faculty and staff; and,
- Foster a culture of wellness and interactive engagement.
 Allen Anandarajah, MDAnandarajah is leading the effort to advance these goals through a methodical process, and actions to date include:
Allen Anandarajah, MDAnandarajah is leading the effort to advance these goals through a methodical process, and actions to date include:
COMPASS Program: During the past year, wellness champions and faculty members from various divisions joined the Colleagues Meeting to Promote and Sustain Satisfaction (COMPASS) Program – an initiative developed by the Mayo Clinic. The sessions promote physician well-being by improving provider engagement, improving meaning in work, and understanding provider needs.
Wellness champions gauged provider feedback on such topics as what matters to them at work, what makes them proud to work here, and what gets in the way of what matters. The divisions that participated were Allergy, Immunology and Rheumatology, Pulmonary and Critical Care Medicine, Nephrology, Hospital Medicine, Palliative Care, Primary Care Network, Hematology/Oncology, and Geriatrics.
Consult etiquette guidelines: The Wellness Committee is working to update and improve etiquette guidelines, which have been in place since 2022. This work appreciates the importance of clear communication in a consult and how consult etiquette can foster physician engagement and promote teaching.
Website: DOM’s Wellness Committee is working to inform colleagues of activities through a dedicated section on the DOM website. The site includes wellness champions, resources, data, and interest groups, such as sporting activities, cooking and music, faculty and APPs can participate in to connect with others. Check it out.
DOM Spotlights Research in Health Equity at Symposium
Tuesday, April 1, 2025
More than 200 people gathered for the Research in Health Equity Symposium to learn about the breadth of community research and engagement efforts.
A highlight of the event was the keynote lecture by sickle cell expert Dr. Wally R. Smith of Virginia Commonwealth University, who also led a dynamic panel discussion with local community advocates.
Check out photos from the event.
Several faculty, staff, and learners were recognized for presenting impactful research:
- Best Community Engagement Project: Wyatte Hall, MA, PhD, (Deaf Wellness Center) and Wyatte Hall, MA, PhD, (Public Health Sciences) for Creating Deaf Equity in Behavioral Health Measurement
- Best Oral Presentation: Ashley Jenkins, MD, (Hospital Medicine) for We Have to Change How We Interact with the Patient: Comprehensive Sickle Cell Care is the Anchor for Ideal Inpatient Sickle Cell Care
- Best Poster Presentation: Milena Insalaco, (Health Equity Research in Oncology [HERO] Lab) for Our Community is Not Appropriately Served: LGBTQ Cancer Survivors and Caregivers Have Suggestions for Providers
- Honorable Mention – Poster Presentation: Laura Perrone, PhD, (Psychiatry Fellow) for UR-Supporting Our Students: Establishing an Expanded School Mental Health Model within the Rochester City School District
Special thanks to the following individuals for coordinating the event: Laura Stamm, PhD, Ahona Shirin, MSPH, and Chunkit Fung, MD, MSCE. We are also grateful to the DOM DEI Council and the Office of Health Equity Research for their support."
Parag Patel Joins QI Scholar Program
Monday, March 31, 2025
 Parag P. Patel, MDParag P. Patel, MD, of Cardiology, was selected for the UR Medicine Quality Institute (QI) Scholar Program to improve healthcare quality and outcomes through collaborative research, teaching and mentoring opportunities.
Parag P. Patel, MDParag P. Patel, MD, of Cardiology, was selected for the UR Medicine Quality Institute (QI) Scholar Program to improve healthcare quality and outcomes through collaborative research, teaching and mentoring opportunities.
As an associate scholar, Patel will connect with faculty across the health system and institution to expand collaborative efforts for quality and performance improvement. This will include gaining priority access to clinical/operational data for analytics, evaluation and research activities, and other QI resources.
“As a physician, I am dedicated to delivering quality care,” said Patel. “The challenge is to build a team and system to operate efficiently while achieving ideal and safe outcomes.”
Efficient care delivery can improve both patient and staff satisfaction while minimizing burnout he said.
“Having experienced the pandemic and the recent IV saline shortage – and seen how staff burnout and accessibility are everyday issues – it’s more important than ever that we learn how to manage the ever-increasing demands on health care and deliver care in a timely manner.”
DEI Roadmap Developed for Meeting Strategic Plan Goals
Monday, March 17, 2025
This is part of a series highlighting the Department of Medicine 2024-2028 Strategy and Action Plan, its five pillars for success, and progress toward meeting the goals.
 The DOM Strategic Plan articulates five focus areas to strengthen our clinical, education, research, workplace culture, and outreach programs. A key mission is diversity, equity and inclusion, and Chunkit Fung, MD, associate chair of DEI, and Laura Stamm, PhD, director of DEI, recently shared an update on how the DOM will meet the goals.
The DOM Strategic Plan articulates five focus areas to strengthen our clinical, education, research, workplace culture, and outreach programs. A key mission is diversity, equity and inclusion, and Chunkit Fung, MD, associate chair of DEI, and Laura Stamm, PhD, director of DEI, recently shared an update on how the DOM will meet the goals.
Three strategic priorities have been identified in a roadmap for implementing the plan: evolving workforce and culture through an inclusive lens, integrating DEI into all missions including community outreach and global endeavors.
The DOM Diversity, Equity and Inclusion Council, which includes DEI champions and a diverse group of APPs, faculty, staff, nurses, fellows and residents, is advising these activities aimed to develop, implement and disseminate initiatives to advance this strategic goal.
Planned activities to evolve the workforce and culture range from establishing a policy on inclusive recruitment and retention processes and initiatives to foster a team that mirrors community demographics. And, an allyship faculty development program will be created, in collaboration with OEI education, to support the effort.
Integrating these goals into clinical, research and education activities will include routine reporting and analysis of clinical metrics by race, ethnicity and gender with development of targets for all divisions.
Faculty collaboration with the URMC Community Advisory Council on initiatives that support increasing under-represented minorities in medicine, provide opportunities for international clinical care and research for our trainees, and offer pathways for selected international medical school graduates to enter our training program.
 Laura Stamm, PhD
Laura Stamm, PhD Chunkit Fung, MD“We are excited to have developed this roadmap for implementing our DEI initiatives,” Fung said. “Our plan includes tangible, achievable actions that will help us reach DOM and URMC’s DEI objectives. Working collaboratively with all divisions and stakeholders across the Medical Center will support these initiatives.”
Chunkit Fung, MD“We are excited to have developed this roadmap for implementing our DEI initiatives,” Fung said. “Our plan includes tangible, achievable actions that will help us reach DOM and URMC’s DEI objectives. Working collaboratively with all divisions and stakeholders across the Medical Center will support these initiatives.”
“First and foremost, our work will be inclusive and transparent,” added Stamm. “We will continue to inform the Department about what we want to accomplish, provide updates on our outcomes and be accountable to the plan.”
Divisions are already working to incorporate DEI activities:
- Hematology/Oncology is enhancing diversity of clinical trial accrual at Wilmot Cancer Institute and fostering more inclusive trial design and development in investigator-initiated trials.
- Palliative Care has been working to specifically include some mention of health care disparity or social justice within didactic sessions.
- Over the last year, the Highland DOM DEI Committee developed a standardized tool to help review root cause analyses from an equity perspective.
- Cardiology developed a Health Equity and Quality Improvement Curriculum by Erica Miller, MD.
Updates on project implementation throughout the divisions are available on the DOM DEI website.
URMC Joins National Network for Bronchiectasis and NTM Care
Friday, March 14, 2025
 Alexandra Adams, MD
Alexandra Adams, MD Sonal Munsiff, MDThe Medical Center is among 33 centers across the country selected for the Bronchiectasis and NTM Care Center Network. URMC was named a Clinical Associate Center, the only site in Upstate New York, supporting specialized care for bronchiectasis and nontuberculous mycobacterial (NTM).
Sonal Munsiff, MDThe Medical Center is among 33 centers across the country selected for the Bronchiectasis and NTM Care Center Network. URMC was named a Clinical Associate Center, the only site in Upstate New York, supporting specialized care for bronchiectasis and nontuberculous mycobacterial (NTM).
Sonal S. Munsiff, MD, of Infectious Diseases, and Alexandra Adams, MD, of Pulmonary Diseases and Critical Care, are co-directors of the center.
“We are proud to be part of the first national network for the treatment of these highly complex lung infections,” said Munsiff. “This national designation is a testament to our leadership in providing outstanding patient care and in conducting cutting-edge research in lung diseases.”
The network aims to develop standards of care that can be implemented across different centers, reduce the diagnosis time and support high-quality care.
“This designation will provide us greater access to clinical research trials to treat these conditions and help improve the standards of care for bronchiectasis and NTM patients across Central and Western New York,” Adams said.
 More than 300,000 people in the United States are treated for bronchiectasis each year. It is characterized by enlarged airways that are thickened or scarred, making it difficult to clear mucus buildup. NTM is a chronic condition caused by mycobacteria and impacts people with compromised immune systems or other lung conditions, like bronchiectasis or COPD.
More than 300,000 people in the United States are treated for bronchiectasis each year. It is characterized by enlarged airways that are thickened or scarred, making it difficult to clear mucus buildup. NTM is a chronic condition caused by mycobacteria and impacts people with compromised immune systems or other lung conditions, like bronchiectasis or COPD.
Network centers will create a national registry of patients, which will help management of the diseases and improve patient outcomes. The teams are working to establish a registry in the EMR to track bronchiectasis and NTM patients and support research.
Strategic Plan: Expanding Access, Innovation to Provide Superior Patient Care
Tuesday, March 4, 2025
This is part of a series highlighting the Department of Medicine 2024-2028 Strategy and Action Plan, its five pillars for success, and progress toward meeting the goals.
 The DOM aims to strengthen its role as "pioneers in superior patient care and public health," as outlined in the strategic plan. Executing this part of the plan focuses on expanding access to care and will build on the Department’s achievements in delivering outstanding patient care. "This pillar of the strategic plan is all about patient access to care,” said Marc Berliant, MD, vice chair for Clinical Affairs. “Through these strategic priorities, we are aiming to increase access to primary and specialty care."
The DOM aims to strengthen its role as "pioneers in superior patient care and public health," as outlined in the strategic plan. Executing this part of the plan focuses on expanding access to care and will build on the Department’s achievements in delivering outstanding patient care. "This pillar of the strategic plan is all about patient access to care,” said Marc Berliant, MD, vice chair for Clinical Affairs. “Through these strategic priorities, we are aiming to increase access to primary and specialty care."
The four priorities are to:
- Deliver world class, equitable care across the Finger Lakes region;
- Leverage modern technology to extend care to all parts of the health system;
- Address social determinants of health; and,
- Disseminate clinical innovation and expertise around the world.

Marc Berliant, MD

Justin Hopkin, MD
One way to improve patient outcome and advance health equity is the Hospital at Home project, which offers promise in enabling patients to be treated at home through provider support and medications, while helping alleviate hospital overcrowding. Care for any conditions -- pneumonia, acute-kidney injury due to dehydration, mild congestive heart failure, COPD and cellulitis – can be provided at home and leaders plan to launch the program this Fall.
"Our multi-stakeholder group is excited to launch this scalable service that will provide better clinical outcomes, enhance patient experience, advance health equity and improve provider well-being," said Justin Hopkin, MD, chief of Hospital Medicine.
Several other programs and initiatives are underway to achieve this strategic pillar’s goals, including:
- Strong Internal Medicine, Highland Family Medicine and the Primary Care Network have joined forces to create a Primary Care Service Line to share best practices and improve quality of care. This service line will be implementing “Making Care Primary,” a CMMI-sponsored model that will compensate PCPs based on quality outcomes. Initial quality metrics include diabetic/hypertension control and colon-cancer screening. This program is one of the Department’s first experiences with a value-based care payment system.
- The Primary Care Network and Strong Internal Medicine are now able to examine clinical outcomes from an equity perspective, to address gaps in care.
- Efforts to leverage technology include utilization of URMC’s new Dragon Ambient Experience (DAX) program. As part of DAX, some DOM providers are using AI to transcribe patient notes.
- The Department is in the process of assessing staffing levels across all divisions to ensure that clinical practices can manage patient volumes. One program that resulted from this assessment is optimizing the use of APPs to provide care in a team-based environment.
- To help improve access in outlying counties, the Allergy, Immunology and Rheumatology team expanded services to Batavia, Geneva General and F.F. Thompson and Infectious Diseases team is establishing consult service and antibiotic stewardship at Geneva General, F.F. Thompson and the Southern Tier.
Sai 'Bindi' Reddy Named Interim Chief of Nephrology Division
Monday, March 3, 2025

Sai Reddy, MD
Clinician-scientist Sai Subhodhini (Bindi) Reddy, MD, has been named interim chief of the Division of Nephrology as chief Thu Le, MD, departs to lead the Department of Medicine at University of California, Irvine. The appointment is effective March 4.
Reddy is clinical director of the division, director of the Strong Memorial Hospital inpatient dialysis and section chief for Highland Hospital Nephrology. She also serves as medical director for the Fresenius dialysis centers in Brighton and Scotts
“I am very pleased Bindi will lead our Nephrology division on an interim basis,” said Ruth O’Regan, MD, chair of Medicine. “Bindi will be an outstanding steward of the division until we identify a permanent chief.”
A national search is underway to identify a new chief.
“It is a privilege to continue in the footsteps of my former predecessors and colleagues, Dr. David Bushinsky and Dr. Thu Le,” said Reddy, professor of Medicine. “I work with an amazing group of people, and I am excited to continue collaborating with them to advance URMC’s missions of delivering excellent patient care, preparing the next generation of clinicians and conducting meaningful research.”
Reddy cares for patients with chronic kidney disease and undergoing dialysis, including pregnant women living with the disease. Her previous research studies included a clinical trial to reduce cardiovascular events in patients with chronic kidney disease and diabetes, and a randomized double-blind trial of peritoneal dialysis exit-site infection prevention.
A past recipient of the National Kidney Foundation’s Excellence in Care Award, Reddy is a member the American Society of Nephrology, Women in Nephrology and the National Kidney Foundation.
Reddy completed her undergraduate studies at Duke in 1989, received her medical degree from Temple University School of Medicine (AOA) in 1993. She began her career at URMC as a medicine resident, later completed a Nephrology fellowship at URMC and then joined the faculty in 1998. Over the years, she has been a member of the faculty senate and faculty professional council.
Research Leadership Team Update
Friday, February 14, 2025
There have been many recent federal policy changes that have left us all with questions and concerns. The Department of Medicine is committed to providing clear, coordinated, and consistent guidance on these changes, in alignment with the University of Rochester.
The University has launched a dedicated website to provide our community with updates and guidance on federal policy changes. The site includes:
- FAQs on research, immigration enforcement, and data privacy and legal protections
- The latest University messages on executive orders and announcements
- Guidance for researchers
- Web form for community members can submit questions.
- A new Policy Updates for Researchers web page
- Additional guidance on immigration enforcement and University protocols, including legal parameters, and rights and responsibilities for students, employees, and University officials when interacting with immigration officers.
You are encouraged to share these resources with colleagues who may receive questions or need this information in their roles.
We will continue to provide updates as we receive them. If you have any questions, concerns or ideas to share, related to recent changes and impacts on research specifically, please reach out to us: Valentina Kutyifa, MD, PhD, Laura Calvi, MD, or Stefanie Fingler (Stefanie_Fingler@URMC.Rochester.edu).
Strategic Plan: Making Progress in Amplifying Excellence in Training and Education
Wednesday, February 5, 2025
This is part of a series highlighting the Department of Medicine 2024-2028 Strategy and Action Plan, its five pillars for success, and progress toward meeting the goals.
 A key element of the Strategic Plan is to train the next generation of academic leaders, physicians and scientists to excel in the evolving healthcare and research systems. Within the Amplify Excellence and Esteem in Training and Education pillar, there are three strategic priorities:
A key element of the Strategic Plan is to train the next generation of academic leaders, physicians and scientists to excel in the evolving healthcare and research systems. Within the Amplify Excellence and Esteem in Training and Education pillar, there are three strategic priorities:
- Build the strongest pipeline to all our missions. Planned actions range from maximizing recruitment for educational programs to increasing retention of trainees and faculty and engaging alumni in recruitment, mentoring and retention of trainees and faculty.
- Support the development of faculty as educators. These efforts include recognizing excellence in teaching, educating and mentoring and supporting engagement in educational activities by promoting faculty wellness.
- Employ a centralized pathway to training, assistance, engagement, mentorship and skill development opportunities for all types of scholarship. Planned actions include centralizing tracking of scholarship outcomes of trainees and junior faculty, disseminating research and scholarship findings, and enabling and promoting opportunities in scholarship and research.

“These strategic priorities are critical to our mission as an academic medical center and to providing the best education for physicians,” said Catherine Gracey, MD, Vice Chair of Education, DOM. “We aim to support scholarship and the development of skills in clinical, translational and basic-science research and in the areas of educational and quality-improvement science. We want to support scholars in their areas of interest.”
To date, work has focused on the recruitment pipeline, alumni engagement and faculty-development activities. The Medicine and Medicine-Pediatrics residencies are in the midst of their annual recruitment, and the DOM fellowship matches were quite successful.
A major upcoming event for alumni engagement is the 100th reunion of the Medicine Residency program, which is planned for the weekend of May 30, 2026. A new alumni newsletter has also been created.
Transitional Care Medicine Transforms Lifelong Patient Care
Wednesday, February 5, 2025
DOM’s Division of Transitional Care Medicine is redefining care for patients with chronic medical or developmental conditions during their transition from adolescence to adulthood. Led by Interim Chief Steven Scofield, MD, and Francis Coyne, MD, director of the Complex Care Center, the division’s collaborative model has resulted in improved care coordination, reduced complications and smoother transitions for patients as they age from pediatric to adult care.
“We have clear evidence that our approach is leading to better health outcomes,” Scofield said. “The division’s comprehensive-care model has reduced ED utilization and improved outcomes for high-risk patients.”

Transitional Care Medicine team
One of its Kind
Many institutions across the country offer transitional care programs and clinics, the Medical Center is the first to establish a dedicated division. This approach provides autonomy, with faculty directly appointed to the division, making transitional care not just a service but a fully integrated academic and clinical entity.
The structure also promotes collaboration across disciplines, enabling specialists from many divisions to work together more effectively, enhancing care for transitioning patients.
Streamlined, Focused Care
On average, physicians get between four and six calls per month to assist patients with intellectual or developmental disabilities who lack the capacity to make their own health care or end-of-life decisions. New York State’s Office for People With Developmental Disabilities requires that two physicians sign off on the Medical Orders for Life-Sustaining Treatment (MOLST) form, in addition to the patient’s parent or guardian. To assist with this process, the division now has three new OPWDD-certified physicians.
Patients with IDD, autism spectrum disorder or behavioral issues face challenges getting services, from dental checkups to routine procedures and surgeries. The Intensive Behavioral Support Team, led by Amanda Laprime, PhD, BCBA-D, LBA, helps screen and desensitize patients before their visits and procedures, which can help reduce staff injury and staff turnover.
Transitional Care’s Applied Behavior Analysis Team is training inpatient nurses caring for patients with IDDs. Offered to Strong and Golisano Children’s Hospital nurses, the training will eventually expand to hospitals across the state.
Research and Education
The division is advancing research in sickle cell care, developing non-hematology expertise to address these patients’ needs. Current clinical trials include the MAYFLOWERS study, evaluating health outcomes of women with cystic fibrosis (CF) on modulators and their babies during and after pregnancy; the STOP-PEDS trial, focusing on optimizing antibiotic use for pediatric CF patients, and the REACH trial, examining disease progression in CF patients who are ineligible for new medications.
A one-year fellowship is offered in transitional care, and resident education spans across Med-Peds, Internal Medicine and Family Medicine. Residents rotate into the Complex Care Center, gaining direct experience with complex conditions and the array of courses, such as the combined Med-Peds/Pulmonary elective, give residents exposure to clinics and provide a foundation in transitional care.
Three Faculty Earn Research, Teaching Awards
Wednesday, February 5, 2025

Brendan Guercia, MD

Erika Drury, MD

Rebecca Levy, MBBCh
Nephrology and Hematology/Oncology faculty were awarded research and teaching grants to advance care and education of the next generation of physicians.
Nephrology’s Rebecca Levy, MBBCh, received the 2025 UR CTSI K12 (formerly KL2) Scholar Award to examine outcomes for adolescents and young adults with chronic kidney disease and explore potential interventions to reduce unnecessary hospitalizations. The award provides 75 percent FTE support for two years.
Erika Drury, MD, of Nephrology, was selected as the 2025-2027 Ritchie Teaching Fellow. She will create a cardiovascular-kidney-metabolic health curriculum for the Nephrology Fellowship. The two-year award provides 10 percent FTE support.
Brendan Guercio, MD, of Hematology/Oncology, received a $250,000 Career Development Award from the Bladder Cancer Advocacy Network (BCAN.) He will investigate whether a healthy diet can help the immune system’s ability to fight advanced bladder cancer when coupled with the newest therapy, enfortumab, vendotin, and pembrolizumab (EVP). Guercio previously won a BCAN Young Investigator Award and has already shown that a nutritious diet enhancing the gut microbiome, along with immunotherapy, may lead to better bladder cancer control.
Morning Report Room Renovation Underway
Tuesday, February 4, 2025
 The long-awaited renovation to the DOM Morning Report room (7.2346/7.2366) is underway. Throughout construction, which is expected to be completed in mid-April, morning reports shifted to the Young Room (3.3235), near to Chair’s suite.
The long-awaited renovation to the DOM Morning Report room (7.2346/7.2366) is underway. Throughout construction, which is expected to be completed in mid-April, morning reports shifted to the Young Room (3.3235), near to Chair’s suite.
The room updates will provide more functional space within the main hospital for clinical work, conferences and meetings. It will also better meet the needs of DOM’s student and residency programs following significant growth over the past two decades.
Specific upgrades will include an updated sound system to enable more interactive hybrid meetings, moveable tables and chairs for room reconfiguration for small or large groups, an additional workstation for residents and learners, a kitchenette and a water cooler.
A special thank-you to Adam Anolik, Medical Center CFO, Mike Rotondo, MD, URMFG CEO, Amber Foster, senior director of Space Planning, and Gerard Mikols, Senior Associate Dean of SMD Finance & Administration, for helping secure project approval.
Many others helped make the renovation possible, including Krista Pike and Katie Murphy of Residency/Fellowship programs; Kate French, of Clinical Administration; Lorie Damann, of Facilities and Karin Staub, of Space Planning, and the Hospital Operations/Space Planning team.
First Pathways Event Held For Medical Students
Wednesday, January 22, 2025
The first DOM Council Pathways event for medical students from various affinity student groups. Turnout was tremendous at this networking dinner, and the students greatly appreciated the opportunity to get together.
Pathways events aim to facilitate mentorship opportunities, enable students to learn about diverse career trajectories, and build a sense of community, belonging and inclusion by having students and mentors engage in a friendly, casual environment.
These events are also a way to help build medical students’ interest in pursuing an Internal Medicine residency at URMC.
Clare Park, DO, and Janice Cheong, MD, organized the January 9 dinner, and another is planned for the spring.



Kari Steinmetz Wins CTSI Shark Tank Funding Competition
Wednesday, January 22, 2025
 CTSI held its Translational Science Shark Tank event in October, with teams developing solutions to seemingly intractable barriers to recruitment in clinical research.
CTSI held its Translational Science Shark Tank event in October, with teams developing solutions to seemingly intractable barriers to recruitment in clinical research.
Kari M. Steinmetz, BA, COA, assistant director of Clinical Trials, and her team, presented creation of an Open Research Round Table Committee to enhance collaboration between research teams and participant recruitment groups. Following the competition, Steinmetz was asked to conceptualize her idea and secured CTSI funding to pursue it.
“With these resources, we aim to eliminate communication barriers that frequently impede clinical-research recruitment” Steinmetz said. “Through a standardized system, we hope to streamline collaboration among research-team members while enhancing participant engagement.”
Communication barriers between researchers and recruitment teams frequently slow the enrollment process in clinical trials, resulting in inefficient recruitment and missed enrollment targets. By identifying barriers to recruitment and discussing potential solutions, the round table committee will help meet research-enrollment targets and better engage research participants.
The committee will consist of coordinators, principal investigators, and study participants, and initially be piloted in Infectious Diseases before expansion across all divisions. The model could also be applied to community engagement, allowing potential participant recruitment groups to contribute ideas.
“My hope is that we can turn this pilot into a long-term project that expands from an internal process to a community effort,” Steinmetz said. “For example, in the community, we could discuss a barrier such as vaccine hesitancy. Researchers would have the opportunity to learn more about the reasons behind this hesitancy and to explain the safety of vaccines.”
Faculty and Staff Artwork Brightens DOM Community Space
Wednesday, January 22, 2025
The DOM Community Space is now home to a variety of pieces or artwork by faculty and staff.
“When we renovated the space, we thought what better way to embody the work of our staff and faculty than to feature their donated artwork,” said Erica Couch, department coordinator, who manages the Community Space at 3.5100.
After last year’s opening, there was an opportunity for artwork submissions and the response was tremendous. Contributors whose artwork and photography on display now are:
- Christopher Nolan, MD, of Pulmonary and Critical Care
- Candice O’Connor, of Infectious Diseases
- Brandon Sprung, MD, of Gastroenterology and Hepatology
- Neil Scheier, MD, of Primary Care
- Deepak Sahasrabudhe, MD, of Hematology/Oncology
- Adelaide Weidner, MS, of Endocrinology, Diabetes and Metabolism
Selected Works

Yosemite Falls, California by Erica Couch, MD

Rose of Sharon by Neil Scheier, MD

A Donated Collection by Brandon Sprung, MD
Can You Guess the Famous Building? by Deepak Sahasrabudhe, MD

Beauty in Hope by Candice O'Connor, MD
"A maiden with PCOS holds her newborn baby next to her partner. She represents hope for reproductive health."
Each piece of art includes a plaque crediting the artist. Plans are to eventually have a rotating art exhibit in the space, likely on an annual basis.
“We are excited that this artwork is now displayed in the Community Space,” Couch added. “It took a bit longer to get everything printed, framed and displayed than we hoped, but we are very happy with how it turned out. We encourage everyone to see the beautiful artwork created by their colleagues.”
The pieces can be viewed daily between 11:30 a.m. and 1:30 p.m. (it requires ID badge access). To gain access outside of the regular hours, contact: erica_couch@urmc.rochester.edu.
Give DOM A Boost Before Doximity Voting Opens for US News Rankings
Wednesday, January 22, 2025
Most DOM clinical faculty are registered on Doximity, the only place where physicians can vote in the annual US News & World Report Best Hospitals survey.
Balloting will begin soon – typically in February and March – and we urge you to start adding colleagues to your network. This move can help boost URMC's reputation in clinical areas for ranking: Cancer, Heart & Heart Surgery, Endocrinology, Gastroenterology, Geriatric Care, Nephrology, and Pulmonary.
When you update your profile, or are mentioned in a publication, everyone in your network gets an update. The more connections you have, the more people who will see URMC/Strong Memorial Hospital. And we hope they’ll think of us come voting time.
All faculty are encouraged to connect with former classmates, physicians you've trained with, and other colleagues to help your division improve its reputation score in the annual rankings!
New Procedures Launched to Bolster Clinical Trials
Wednesday, January 22, 2025
A new standard operating procedure (SOP) for Department of Medicine investigators was recently introduced to ensure feasibility of clinical trials as part of a new, comprehensive clinical trials platform. Its primary mission is to achieve translation through clinical trials, with the goal of creating a uniformed framework to identify innovative studies that align with the missions of DOM’s various divisions.
“We are launching a novel, innovative clinical trials framework to promote a strategic, managed clinical trials portfolio, effective trial operations and diversity, in alignment with the DOM Strategic Plan,” said Valentina Kutyifa, MD, PhD, vice chair for Clinical Research. “Most importantly, processes for start-up, feasibility, and conduct of clinical trials are being harmonized and modernized across our divisions to set up our investigators for success.”
With this streamlined process, new studies will be identified that are feasible and advance the institution’s strategic priorities. Last week, URMC CEO David Linehan, MD, cited his goal of building an “absolute powerhouse for clinical trials and clinical investigations.”
The DOM is at the forefront of this effort, with more than $247.7 million in research funding is the largest across SMD. This is the first of the DOM Clinical Trials Umbrella procedures aiming to achieve these goals.
The SOP’s scope covers clinical research protocols that prospectively enroll randomized and non-randomized human subjects, including sponsored and investigator-initiated research, clinical trials and FDA-regulated studies.
Key elements of the new DOM clinical trials framework include a Clinical Research Leadership Committee, harmonized organizational structure and mission statement, harmonized use of OnCore across divisions, a Protocol Review Committee and enhancing study start-up activities including IRB support. Other elements include advancing the use of e-consent and electronic study documentation, ongoing feasibility review, PI engagement, improved oversight and training, and competitive staff recruitment, training and retention.
The feasibility assessment of new clinical trials encompasses seven steps: sponsor inquiry, go/no go check, completion of a new, standardized feasibility worksheet, formal risk assessment through OCR, score calculation, protocol review by the DOM Protocol Review Committee and decision.
The next initiative is focusing on harmonizing the use of OnCore across all divisions. DOM hopes to soon implement its usage in all studies, currently at about 80 percent for DOM sponsored studies across all divisions.
“This SOP marks the beginning of a unified approach across all 15 divisions of medicine, providing a clear framework to align clinical trials with our strategic goals and ensuring swift and successful execution of studies that drive our mission forward,” said Stefanie Fingler, MBA, director of Research Operations.
Kari Steinmetz, MBA, assistant director of Clinical Trials, said, “With almost three decades of experience across various departments at the University of Rochester, I’ve seen firsthand how clear, consistent and well-communicated SOPs can serve as a vital tool in driving efficiency, consistency and quality across all levels of an organization. This SOP will help us reduce inefficiencies, foster communication and ultimately drive the success of our organization.”
The new SOP is a pilot that will be evaluated at the end of the year. For questions, contact the Research Leadership team.
URMC Department of Medicine Clinical Trials Framework
Jennifer Anolik Named Chief of Allergy, Immunology and Rheumatology Division
Monday, January 6, 2025
 Internationally renowned physician scientist Jennifer H. Anolik, MD, PhD, was named chief of the Allergy, Immunology and Rheumatology (AIR) Division in the Department of Medicine, after serving as interim chief since 2021.
Internationally renowned physician scientist Jennifer H. Anolik, MD, PhD, was named chief of the Allergy, Immunology and Rheumatology (AIR) Division in the Department of Medicine, after serving as interim chief since 2021.
“I am delighted that Jen has agreed to continue leading our AIR division as chief,” said Ruth O’Regan, MD, chair of Medicine. “The division is in great hands under her leadership and will continue to benefit from her experience and expertise as a clinician, educator and researcher. I am extremely grateful to her for serving as interim chair over the past few years.”
A faculty member for 22 years, Anolik also serves as associate chair for research in the Department of Medicine, professor of Medicine, Pathology, and Microbiology and Immunology, and director of the Internal Medicine Physician Scientist Training Program.
Anolik earned her MD and PhD at the University, completed her residency in Internal Medicine in 1999 and her fellowship in Rheumatology in 2002, after which she joined the faculty.