Projects
 Developing Therapeutic Strategies to Inhibit Remodeling and Improve Vision
Developing Therapeutic Strategies to Inhibit Remodeling and Improve Vision
We have developed and tested three different approaches to target and inhibit Retinoic Acid-dependent signaling in the degenerating retina, demonstrating reduced spontaneous hyperactivity in RGCs, increased signal to noise ratio in retinal light responses, improved light perception and enhanced contrast sensitivity.
These include:
- Gene therapy delivering a dominant-negative form of the Retinoic Acid Receptor using intravitreal or intravenous viral vectors (AAV2 and AAV9, respectively). [Telias et al., Neuron, 2019].
- Small molecule pharmacological therapy using the inverse agonist BMS-493 delivered via intravitreal injections. [Telias et al., Neuron, 2019].
- Repurposing the ALDH inhibitor Disulfiram to reduce Retinoic Acid synthesis, delivered systemically (per os). [Telias et al., bioRxiv, 2021].
We test the therapeutic potentials of these approaches by implementing ex-vivo molecular and physiological measurements and in-vivo behavioral assays in mice with progressive retinal degeneration.
We are currently:
- Developing new ways of inhibiting the Retinoic Acid Receptor in the retina without affecting its function outside of the retina and in healthy (non-remodeled) RGCs.
- Studying and testing new drug targets that are part of the Retinoic Acid-dependent signaling mechanism responsible for pathological RGC hyperactivity.
- Innovating new assays aimed at testing and measuring the different phenomena associated with inner retinal remodeling.
 Identifying and Characterizing Molecular Markers for Diagnosis and Treatments
Identifying and Characterizing Molecular Markers for Diagnosis and Treatments
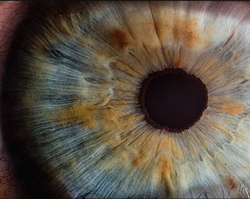
Retinoic Acid-dependent signaling in the inner retinal neurons of mice suffering from degenerative blindness leads to morphological remodeling (Lin et al., FASEB, 2012), spontaneous neuronal hyperactivity and membrane hyperpermeability (Telias et al., Neuron, 2019), and impaired vision (Telias et al., bioRxiv, 2021). Yet, the precise molecular mechanism that follows the activation of RA-signaling is still unknown. Understanding which genes are activated by RA, and how these genes might differ in specific retinal neurons subtypes, will give us a much deeper scientific understanding of how remodeling affects vision as well as potentially provide us with molecular markers that can better identify the different stages of remodeling as degeneration progresses.
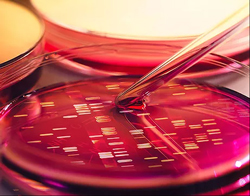
We are specifically interested in the potential involvement of non-coding RNAs, including microRNAs (miRNAs), whose expression is regulated by RA-dependent signals. miRNAs can be found inside secreted vesicles known as exosomes, which are present in the vitreous humor of mice, rats and humans. Our goal is to isolate, characterize and identify these RNA species with the hope of isolating specific sequences that can be used as diagnostic tools.
In order to understand how similar activation of RA affects neurons in a differential way, we combine in-vivo and ex-vivo studies with advanced fluorescence-assisted cell-sorting, single-cell RNAseq and bioinformatic tools. The contribution of individual components in the RA-cascade is tested and measured using ex-vivo single-cell patch-clamp electrophysiology and extracellular multielectrode array recordings.
 Understanding Pathological Signal-Processing Corruption in Mouse and Human Neurons
Understanding Pathological Signal-Processing Corruption in Mouse and Human Neurons
Vision is corrupted by RA-dependent remodeling (Telias et al., bioRxiv, 2021). However, the specific physiological effects of RA, and how they contribute to the overall spontaneous hyperactivity observed in degenerated retinas, is still unknown.
Our goal is to implement a combination of morphological analysis, Calcium-imaging and electrophysiological recordings on single retinal neurons using powerful measuring tools that can generate thousands of data points for individual retinas. These data are then incorporated into computational models that are able to project and even predict the extent of remodeling from individual neurons to complete retinal circuits.