Huxlin, MacRae and URMC colleagues discover a new approach to treat established corneal fibrosis
Monday, October 23, 2023
 The cornea is the clear window at the front of the eye that focuses light onto the retina, enabling “vision” as we know and experience it. Infections, injury and surgery to the cornea can induce a healing response that reduces its clarity. These are leading causes of vision loss worldwide. For the last two decades, Krystel Huxlin, Ph.D., the James V. Aquavella Professor of Ophthalmology at FEI, has explored how to prevent corneal scarring after injury. Now, she and her team have discovered a novel approach to treating already established opaque corneas.
The cornea is the clear window at the front of the eye that focuses light onto the retina, enabling “vision” as we know and experience it. Infections, injury and surgery to the cornea can induce a healing response that reduces its clarity. These are leading causes of vision loss worldwide. For the last two decades, Krystel Huxlin, Ph.D., the James V. Aquavella Professor of Ophthalmology at FEI, has explored how to prevent corneal scarring after injury. Now, she and her team have discovered a novel approach to treating already established opaque corneas.
“Simply stated, healing can cause transparent corneal cells to become opaque, blocking light from reaching the retina, where it should be detected,” Huxlin said. “This transformation is defined by a series of complex events that cause corneal cells to change into myofibroblasts. As our understanding of this process has grown, we have been able to isolate key areas where we can intervene to prevent transformation. However, patients often present to the clinic after opacity and scarring have already occurred. Our lab is one of the first to ask whether it is possible to treat established fibrosis without toxic side-effects.”
A recently published paper in Investigative Ophthalmology & Visual Science, explains this concept and offers a new solution. The team performing the research included Huxlin, FEI research assistant professor Kye-Im Jeon, Ph.D., FEI cornea specialist and refractive surgeon Scott MacRae, M.D., and URMC Department of Medicine bioenergetics expert Keith Nehrke, Ph.D.
 When an injury happens to the cornea, normally quiet cells called keratocytes become activated, changing into fibroblasts, and ultimately, myofibroblasts. The latter are responsible for stabilizing and repairing the wounded corneal tissue, but they are also key components of corneal scars. Many teams, including Huxlin’s, have explored ways to prevent fibrosis, which leads to scarring. This included researching methods of blocking the action of small proteins, including transforming growth factor beta, which regulate how keratocytes transform into myofibroblasts. Although these treatments can be effective, they are limited by the fact that they have to be applied immediately after injury, they cannot reverse existing fibrosis, and they can have unwanted side-effects.
When an injury happens to the cornea, normally quiet cells called keratocytes become activated, changing into fibroblasts, and ultimately, myofibroblasts. The latter are responsible for stabilizing and repairing the wounded corneal tissue, but they are also key components of corneal scars. Many teams, including Huxlin’s, have explored ways to prevent fibrosis, which leads to scarring. This included researching methods of blocking the action of small proteins, including transforming growth factor beta, which regulate how keratocytes transform into myofibroblasts. Although these treatments can be effective, they are limited by the fact that they have to be applied immediately after injury, they cannot reverse existing fibrosis, and they can have unwanted side-effects.
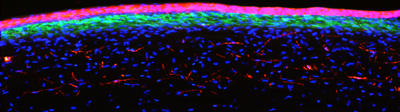
Huxlin and her colleagues’ new work demonstrates feasibility of a completely novel approach to the problem: manipulating a key organelle inside existing myofibroblasts, causing them to revert back to more quiescent cells. To accomplish this, the team introduced a class of compounds, called thiazolidinediones (TZD) into in vitro and in-vivo models of fibrosis. The living model involved exposing the cornea to TZDs weeks after an injury, after fibrosis had occurred. The team’s experiments showed that a particular TZD caused myofibroblasts to lose all of their defining molecular and morphological characteristics, and take on the shape and behavior of more quiescent corneal cells.
The key organelles targeted by the TZD inside myofibroblasts were mitochondria, best known for generating most of a cell’s energy and the signals used to carry out its essential functions. Thanks to the discoveries of our URMC team, mitochondria can now also be thought of as key to powering the ability of corneal myofibroblasts to remain myofibroblasts – knowledge that can be exploited to treat corneal fibrosis.
Although more needs to be understood about the effects of TZDs on myofibroblasts--such as the duration of the effect and the optimal time to apply the treatment--it represents an important step in treating corneal injuries and potentially reversing existing damage. A clinically-viable treatment would prove especially useful in regions of the world where months, even years, may pass before a patient can receive care.
Read More: Huxlin, MacRae and URMC colleagues discover a new approach to treat established corneal fibrosis