About the Program
 Drs Amber Edwards and Bart Simon after winning the Cardiothoracic Surgery Jeopardy World Championship at the 55th STS Annual Meeting in 2019. In the photo from left to right Dr Clauden Louis (’22), Dr. Robert Cerfolio (University of Rochester School of Medicine alumnus ’88), Dr Amber Melvin (’19), Dr Bart Simon (’22), Dr Katherine Wood (’20), Dr George Hicks (former program director and U of R School of Medicine and CT alumnus ’79)
Drs Amber Edwards and Bart Simon after winning the Cardiothoracic Surgery Jeopardy World Championship at the 55th STS Annual Meeting in 2019. In the photo from left to right Dr Clauden Louis (’22), Dr. Robert Cerfolio (University of Rochester School of Medicine alumnus ’88), Dr Amber Melvin (’19), Dr Bart Simon (’22), Dr Katherine Wood (’20), Dr George Hicks (former program director and U of R School of Medicine and CT alumnus ’79)
Our Program Focus
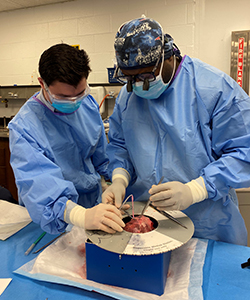
Dr. Clauden Louis (’22) when chief resident and a medical student
during a coronary bypass simulation lab
- Residents receive training of the highest caliber by dedicated Cardiac and Thoracic Surgery faculty from the University of Rochester that are strongly committed to preparing trainees for clinical practice as well as developing skills in teaching, research and leadership for their future careers.
- Training takes place at the University of Rochester Medical Center, a quaternary, academic hospital servicing all of upstate New York. As the premiere medical center in the region, we are fortunate to have robust clinical volumes in all aspects of cardiothoracic surgery and have developed rich programs in valvular heart disease, heart failure and mechanical circulatory support, congenital heart disease, thoracic surgical oncology and benign esophageal disease.
- The faculty are focused on minimally invasive approaches to all aspect of adult cardiac and thoracic surgery including endovascular and mini-transthoracic approaches to valvular heart disease, non-sternotomy approaches to ventricular assist device insertion, endoscopic approaches to benign and malignant esophageal disease and utilization of robotic, VATS or laparoscopic techniques in nearly every major thoracic case.
- Progressive responsibility at all levels, with emphasis placed on academic knowledge and technical advancement for the development of expertise in patient care.
Program Highlights
Our Training Model
We are dedicated to the integrated six-year (I6) training paradigm as our program was one of the first to adopt this cutting-edge model of training the next generation of cardiothoracic surgeons graduating our first resident in 2016.
Our program is uniquely equipped to offer robust opportunities in every area of Cardiothoracic Surgery; including Adult Cardiac, Congenital, Heart Failure and Mechanical Circulatory Support, Transplantation, General Thoracic and Esophageal Surgery.

Chief of Thoracic and Foregut Surgery, Dr. Jones,
with PGY1 Ariana Goodman and PGY2 Nick Searcy during a Lobectomy simulation lab
Technology
Residents at University of Rochester are exposed to, and trained in the use of the latest cutting edge technology. We have a robust minimally invasive structural heart practice spearheaded that includes minimally invasive and endovascular valve replacements. The Mechanical Circulatory Support program at URMC is a national leader in left ventricular assist devices (LVAD), minimally invasive LVADs, and extracorporeal membrane oxygenation (ECMO). Residents will learn novel approaches to aortic surgery (TEVAR, EVAR), off pump coronary surgery, minimally invasive procedures and innovative techniques in the treatment of congenital heart disease in neonates and adults.
Esophageal Diagnostic Laboratory
Unique to the University of Rochester, the Esophageal Diagnostic and Endoscopic Laboratory is a state of the art facility for the diagnosis and treatment of esophageal disorders run by the Thoracic surgical faculty. Diagnostic techniques such as upper endoscopy, high resolution manometry, and pH monitoring can be performed right in the clinic. We also perform advanced endoscopic techniques including esophageal dilation and stenting, endoscopic mucosal resection (EMR) and radiofrequency ablation and per oral endoscopic myotomy (POEM). We have an outstanding research program investigating advanced diagnostics, treatment strategies, and outcomes research of esophageal disease. Time in the lab is incorporated when rotating on the thoracic surgery service. For those residents who wish to focus on thoracic surgery, there is a dedicated rotation during the third year.

Dr. Bart Simon (’22) presents his research at AATS annual meeting in 2019
Cardiology Collaboration
Residents on the Cardiac focused track will rotate in the Cardiac Catheterization and Echocardiography laboratories during their third year of training. The Cardiac Catheterization lab rotation is designed to provide experience in diagnostic coronary angiography and gain familiarity with catheter based approaches to coronary disease, congenital lesions, heart biopsies, invasive hemodynamics, and arrhythmias. As Senior residents, trainees are performing transcatheter valves and other endovascular interventions supervised by Cardiac Surgery and Interventional Cardiology faculty who work collaboratively in the care of patients. The echocardiography rotation exposes the resident to acute and chronic cardiovascular problems both through direct patient imaging and through many formal and informal didactic teaching sessions. Residents build a foundational experience in both transthoracic and transesophageal imaging techniques and interpretation essential to the practice of Cardiac Surgery.
Research
Residents are encouraged to participate in research and publish with the faculty.
Frequently Asked Questions
October 11, 2024
One position per year.
We receive approximately 130 applications a year.
Selected applicants will be notified by email on October 22, 2024, the universal offer date for thoracic residency programs.
Yes, we were one of the first programs to go through the 10 year ACGME accreditation cycle.
No, but highly encouraged. A research year is not mandatory but is offered for those interested in spending a dedicated year in academic pursuits.
The progressive growth of the resident into a Cardiothoracic surgeon is expected to develop in a step wise fashion through a graded level of independence, authority, and responsibility from the early development of skill sets both technical and cognitive with the goal of achieving proficiency in all aspects of patient care and personal growth. The resident will progress from first assistant to primary surgeon over the course of the training program.
Moonlighting is not allowed when on service.