PGY2 Oncology
Welcome
Welcome and thank you for your interest in our PGY-2 Oncology Pharmacy Residency program at the University of Rochester Medical Center. As a program, we aim to provide the resident with a diverse clinical experience in both inpatient and outpatient oncology, and provide quality educational opportunities, in a supportive working environment. Our residency program has highly qualified and dedicated preceptors, many of which are board certified. As our PGY-2 resident you will be integrated into our multidisciplinary teams and will have the opportunity to work with passionate and devoted professionals.
On behalf of all of our preceptors, we truly appreciate your interest in our program at URMC and we look forward to meeting you!
Our Program By the Numbers
9
8
+
10
85
+
At a Glance
Program Curriculum
Our full-time curriculum provides the essential elements needed to mold a well-rounded clinical pharmacist.

Resident Well-Being
Burnout is real. Our longitudinal programming on building resilience, finding work-life balance, and managing stress is one of the reasons residents recommend URMC.
Life of a Resident
Our emphasis on work/life balance is an important reason fellows choose URMC. A focus on trainees' well-being enables you to learn and thrive in Rochester.
Program Details
Meet our PGY2 Oncology Resident, Deidra, and Go on a Tour of the Inpatient Oncology Areas!
*Last updated 2020-2021
Tour Additional Oncology Areas of the Hospital
*Last updated 2020-2021
The PGY2 Oncology Pharmacy Residency at UR Strong Memorial Hospital Wilmot Cancer Institute is a 12-month, full-time curriculum that provides the essential elements needed to shape a successful pharmacy specialist. This intensive training involves activities in a wide variety of practice settings.
- Rounding with multidisciplinary malignant hematology, medical oncology and blood/marrow transplant clinical teams
- Providing ambulatory pharmacy services to both patients with solid tumors and hematologic malignancies in the outpatient Wilmot Cancer Institute clinics
- Providing direct pharmaceutical care to patients enrolled in clinical research studies
- Participating in the oral chemotherapy program by providing patient education, clinical follow-up and drug information services
- Applying appropriate sterile compounding technique for chemotherapy preparation
- Precepting, counseling, and teaching patients, students, residents, pharmacists, advanced practice providers and oncologists, serving as an integral part of the healthcare team
Rotation Schedule
The schedule for the residency year is outlined below and is tailored to meet the needs and interests of the individual resident.
Core Rotations (Required)
- Orientation (2 weeks)
- Chemotherapy Drug Preparation & Outpatient Infusion Center (MTC) (4 weeks)
- Inpatient Solid Tumor Oncology (3 weeks)
- Inpatient Malignant Hematology (6 weeks)
- Inpatient Blood and Marrow Transplant & Cellular Therapy (5 weeks)
- Outpatient Oncology - Breast and Gynecologic Oncology (4 weeks)
- Outpatient Oncology - Gastrointestinal, Neuro, and Sarcoma (4 weeks)
- Outpatient Oncology - Genitourinary, Thoracic, and Melanoma (5 weeks)
- Outpatient Oncology - Lymphoma (3 weeks)
- Outpatient Oncology - Leukemia (3 weeks)
- Outpatient Oncology - Myeloma and Benign Hematology (3 weeks)
Longitudinal Rotations (Required)
- Projects, Presentations, and Preceptorship
- Geriatric Oncology Clinic
- Research
- Management and Leadership
- Investigational Drug Service
- Staffing and Operations
Elective Rotations
Elective rotations are designed to customize the oncology residency experience in order to fit the needs and desires of each resident. The PGY2 Oncology rotation schedule allows for two 3-week elective learning experiences.
- Benign Hematology
- Pharmacy Management
- Specialty Pharmacy
- Pain and Palliative Care
- Pediatric Hematology/Oncology
- Transplant Infectious Diseases
- Investigational Drug Service
- Advanced (Concentrated) Core Learning Experience
Additional Opportunities and Research
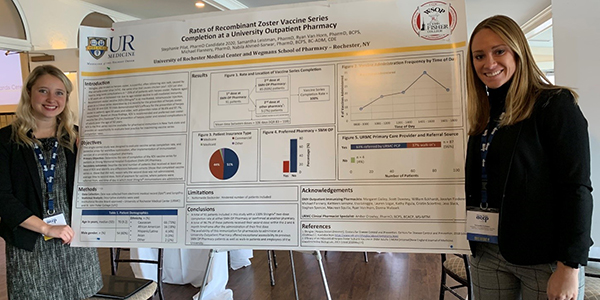
- Research – The resident will complete a major research project during the residency year. Research project results will be presented at the Hematology/Oncology Pharmacy Association (HOPA) Annual Conference and submitted for publication.
- Presentations – The resident will have opportunities to develop teaching skills by developing and delivering presentations to various audiences, including pharmacy staff, pharmacy students, residents, nurses, and hematology/oncology fellows.
- Advancing Clinical Practice – The resident will have opportunities for developing and reviewing Beacon treatment plans, oncology-relevant institutional protocols, and formulary reviews at the Oncology Pharmacy & Therapeutics Subcommittee meetings.
- Resident Learning Series (RLS) – Preceptors, oncology pharmacists, residents, students, and other guests meet during this weekly pharmacy conference designed to facilitate learning on various oncology-related topics throughout the year. The format of RLS varies between lectures from preceptors on specific disease state treatments, journal clubs reviewing primary literature, and informal topic discussions.
- Meeting Attendance – The resident will receive funding to attend the HOPA Annual Conference meeting (required), the NYS ACCP Annual Meeting (optional), and UB Resident Research Day (required).
Resident Well-Being
Life of a Resident
Here is a typical inpatient day:
- 6:30 a.m. Arrive to the hospital to work-up patients for rounds.
- 8:00 a.m. Pre-round with preceptor to discuss recommendations and plan for patients.
- 8:30 a.m. Round on inpatients with interdisciplinary team.
- 12:00 p.m. Grab lunch with co-residents and follow-up with any patient care needed.
- 1:00 p.m. Meet with preceptor for topic discussion/literature review or attend any meetings/conferences.
- 2:00 p.m. Ensure chemotherapy admissions’ orders are completed and ready to begin if not started in the morning.
- 3:00 p.m. Follow-up with team regarding patient care.
- 4:00 p.m. Update preceptor about any changes in patient care.
- 5:00 p.m. Head home and enjoy Rochester!
*Schedule will vary depending on the rotation the resident is on during the year.

Purpose Statement
PGY2 pharmacy residency programs build on Doctor of Pharmacy (Pharm.D.) education and PGY1 pharmacy residency programs to contribute to the development of clinical pharmacists in specialized areas of practice. PGY2 residencies provide residents with opportunities to function independently as practitioners by conceptualizing and integrating accumulated experience and knowledge and incorporating both into the provision of patient care or other advanced practice settings. Residents who successfully complete an accredited PGY2 pharmacy residency are prepared for advanced patient care, academic, or other specialized positions, along with board certification.
This PGY2 advanced pharmacy practice residency program in oncology is intended to develop the knowledge, skills and abilities of a qualified pharmacist that are necessary to be an expert clinical pharmacy practitioner in oncology. It is intended that a graduate of this program will be fully qualified to develop and sustain an independent and successful clinical pharmacy practice in any oncology setting.
We place tremendous value on resident well-being and offer a longitudinal series which helps our residents achieve a better work-life balance. We strive to provide our residents with the skills they need to manage their stress and build resilience, not only for residency training, but for their professional careers.
Sessions incorporate guest speakers, various icebreaker activities, events such as preceptor-resident get-togethers, and lots of fun!
Topics covered include:
- Understanding Wellness, Resilience, and Burnout
- Developing Self-Care Strategies as a Resident
- Understand Factors That Can Contribute to Burnout
- Handling Conflict and Difficult Conversations
- Creating a Culture of Resident Well-Being
What Our Graduates Are Saying...

"I strongly value the importance of training in a different town/state than where someone pursues his/her degree, so I knew I wanted to leave Pennsylvania for PGY2. Not only would this strengthen my pharmacy knowledge, but hopefully I would be able to extend some things I have learned throughout my schooling/PGY1 to ultimately provide the best care for patients! Ultimately, I chose URMC for the diverse opportunities in hematology/oncology in both the inpatient and outpatient/specialty settings. During my interview, I immediately felt the inviting atmosphere within the Pharmacy Department. There was a true sense of community and support that radiated from the strong leadership that solidified my desire to be a member of this incredible team! It is also a plus that I am really loving the Rochester area as well!"
Deidra Smith, PharmD
PGY2 Oncology
Class of 2020-2021
Contact Us
Bryan Fitzgerald, PharmD, BCOP
Director | PGY2 Oncology Pharmacy Residency Program
Oncology Clinical Pharmacy Specialist
University of Rochester Medical Center
601 Elmwood Ave, Box 617
Rochester, NY 14642
Phone: (585) 273-4767
The information contained herein is subject to change. Please feel free to contact the residency program directly for the most up-to-date information and/or other residency related questions.
