VIP-SMI Study

Vertical Integration for Patients with SMI (VIP-SMI):
This patient-centered transitions in care study is funded by the University of Rochester Medical Faculty Group and the University of Rochester Quality Institute’s innovation grant award.
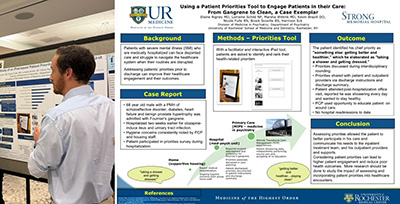
The intervention includes a point-of care iPad-based prioritization tool to help patients identify and communicate their health-related priorities prior to discharge (Project 1), and expands the reach of an existing Transitional Care Management (TCM) program via systematization of the work of “comprehensivist clinicians” who provide a bridge between the hospitalist and primary care teams (Project 2).
Intervention activities include individualized pre-discharge and post-discharge processes aimed at supporting and engaging patients in transitions back to the community.
Background:
Preventable hospital readmissions are a costly burden on our health system which is already taxed by clinician shortages and burnout related to the COVID pandemic. For patients, readmissions are a source of disappointment, and lead to worse health outcomes. Many readmissions can be traced back to the arbitrary boundaries of our siloed medical system, in which breakdowns in communication and coordination between inpatient and outpatient care are rampant. For patients with concomitant medical and psychiatric needs the challenges are particularly daunting, especially among the most vulnerable patients with severe mental illnesses (SMI) who may also face housing and food insecurity, stigma and trauma, further complicating their transitions of care. These complications often leave vulnerable patients with SMI disenfranchised and they are rarely given the chance to participate in prioritizing their own needs when it comes to discharge planning.
The novel Medicine in Psychiatry Services (MIPS) at the University of Rochester Medical Center were created within the department of psychiatry to breakdown the silos of medical (physical) and psychiatric (mental health) care which often prevent people with SMI from accessing the kind of quality medical care they deserve. MIPS – which includes both a primary care practice and two inpatient units - is perched at the crossroads of the medical and psychiatric health sectors, as well as primary and acute care.
Over the last two years, reducing medical readmissions has become a priority for both the Medicine in Psychiatry Primary Care (MIPS-PC) and Inpatient Medicine in Psychiatry (IMIP) settings, yet efforts have not been well integrated across these settings. Although several clinicians work in both IMIP and MIPS-PC, their cross-system expertise has not been systematically utilized. This past year, MIPS was formally recognized by the department of psychiatry as a division and supported to develop common leadership and priorities. This has presented MIPS with a new opportunity to restructure care to achieve outcomes that are important to both patients and the various health systems that serve them.
In order to reduce costly medical readmissions for patients with SMI, we will incorporate emerging health services innovations known as vertical integration and comprehensivist care, which call for integrating care and clinical personnel across inpatient and outpatient settings, and have demonstrated success for reducing medical readmissions. The vertical integration intervention will additionally maximize the electronic medical record to include patient identified priorities as part of standard operating procedures. Furthermore, we will incorporate key domains identified in the literature as effective for reducing readmission rates for vulnerable patients. We will then test whether the intervention improves healthcare utilization via reduced seven and thirty-day medical readmission rates. In addition, we will explore whether the intervention improves primary care engagement in the two weeks post discharge.
We hypothesize that patients who are discharged from MIPS during the intervention will be less likely to be readmitted than case-matched patients who are either discharged from comparable non-MIPS units during the same period or discharged from 19200 (MIPS unit) during the pre-intervention period. We further hypothesize that MIPS-PC patients who are discharged from IMIP during the intervention phase will have a higher rate of follow up in the clinic in the two weeks after discharge than MIPS primary care patients who are discharged prior to the intervention implementation.