Post-hospitalization Improvements in Transition (PHIT)
 Clinical and research leaders are working collaboratively to develop and evaluate an intensive, patient-centered approach to transitioning patient care from the hospital to the community.
Clinical and research leaders are working collaboratively to develop and evaluate an intensive, patient-centered approach to transitioning patient care from the hospital to the community.
The project will focus on integrating proactive psychological services into the daily work-flow of a medical unit.
Primary goals will be to assess the effectiveness of a program aimed at:
- Expedited triage of mental health assessments including suicide risk
- Development of a patient-centered discharge transition program
Background
Patients with Serious Mental Illnesses face significant health disparities due to poorly coordinated care.
Serious mental illness (SMI) is defined as a mental, behavioral, or emotional disorder resulting in serious functional impairment, which substantially interferes with or limits one or more major life activities. People with SMI die 15-30 years earlier than others. Much of the mortality gap can be attributed to poorly coordinated medical and psychiatric care. Patients with SMI are more likely to face challenges managing chronic medical illness due to behavioral impediments and inadequate psychosocial support. Integrated medicine and psychiatry services that are targeted to patients' circumstances and priorities have the potential to improve patients’ quality of life and reduce the mortality differential.
Patient with Serious Mental Illnesses incur high costs for the US health systems due to poorly coordinated care When care is poorly coordinated it leads to inefficiencies such as frequent emergency room visits, increased lengths of stay and frequent re-admissions to the hospital. Patients with SMI are among the 5% of patients who account for nearly 50% of the health care costs in the US, aka “high needs-high cost patients”.
The unique integrated clinical services within the department of Psychiatry are well positioned to be on the cutting edge of healthcare redesign. The Medicine in Psychiatry Primary Care Clinic and the inpatient Medicine in Psychiatry unit have been operating at the University of Rochester for a decade. Both clinical sites have been developing medical services targeted to patients with SMI.
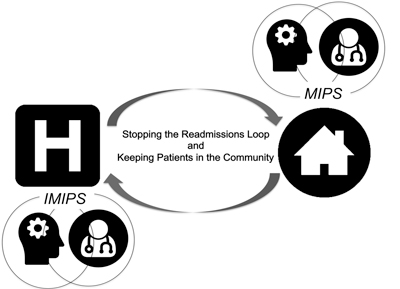
For this project, we plan to focus our efforts on improving integration between medical and behavioral health services and collaboration across inpatient and outpatient settings. IMIP has recently taken on several quality improvement projects to determine best practices for patients with SMI and acute medical needs. This has led us to explore more explicitly when and how integration should occur. For example, in order to address the significant behavioral health needs of patients admitted to the unit for acute medical needs, IMIP has recently partnered with the psychology internship program run through the department of psychiatry. Over the last 2 years, faculty and interns from the psychology internship program have helped unit leadership assess ways of incorporating psychological services into routine care. In addition, starting in July 2018, IMIP has embraced a more proactive model of incorporating psychiatric services with the hiring of a staff psychiatrist who can spend some time 4 hours a week rounding with medical staff on high risk IMIP patients. This is in contrast to the previous consultation model wherein psychiatric services were formally requested after patients’ medical needs were addressed. In addition, there have been several new initiatives to coordinate care between IMIP and MIPS-PCC using care-coordination services.
Project Overview
Proactive psychology assessments:
Partnering with the psychology internship program located in the department of Psychiatry, a needs assessment conducted in led to a new pilot psychology internship opportunity that serves to provide education to psychology interns interested in integrated care, while also providing behavioral health education to IMIP unit staff and assisting the medical team with behavioral health assessments and plans. With careful review of the behavioral health needs of patients and providers, several key areas of opportunity were identified, including the critically important role psychologists could provide for conducting suicide risk assessments. While this assessment would not replace the need for more thorough psychiatric evaluation, it could help make critical decisions to reduce the need for bedside sitters and determine the need (triage) for targeted psychiatric evaluation.
Patient-centered discharge transitions assessment:
The goal of this project is to build on previous research focused on incorporating patient priorities into routine medical care, and ongoing developments to reduce re-admissions among MIPS-PCC patients.
The goal will be to capitalize on psychology services to conduct brief bedside interviews with patients to help assess patient readiness for discharge and explore the patient’s beliefs about what has previously been a hindrance in maintaining health in the community. The information collected in the patient interview will be incorporated- as the patient’s voice- into unit discharge planning meetings.
Key clinical collaborators
Heather Jackson, RN Nurse Manager unit 19200
Lorraine Schild, Lead NP unit 19200
Telva Olivares, Director MIPS