Joint Aspiration
What is joint aspiration?
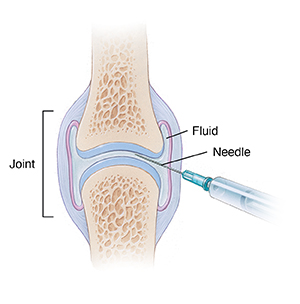
Joint aspiration is a procedure to remove fluid from the space around a joint. It
is done using a needle and syringe. This is often done to relieve swelling or to get
fluid for analysis to diagnose a joint disorder or problem. It may be done with a
local anesthetic to reduce pain.
Joint aspiration is most often done on the knee. But fluid can also be removed from
other joints. These include the hip, ankle, shoulder, elbow, and wrist joints.
Other related procedures may be used to help diagnose joint problems. These include
X-ray, bone scan, MRI, CT scan, arthroscopy, and arthrography.
Why might I need a joint aspiration?
Joint aspiration may be done to diagnose and help treat joint problems. These conditions
may be diagnosed by testing the fluid:
Joint aspiration can also be done to remove a large amount of fluid around a joint.
Sometimes bursitis (inflammation of the bursa) causes fluid to collect near a joint.
Removing the fluid will decrease the pressure. It can relieve pain and improve movement
of the joint. A medicine may be injected after removal of the fluid. This is done
to help treat tendonitis or bursitis.
There may be other reasons for your healthcare provider to advise a joint aspiration.
What are the risks of a joint aspiration?
All procedures have risks. The risks of this procedure include:
-
Discomfort at the aspiration site
-
Bruising at the aspiration site
-
Swelling at the aspiration site
-
Infection at the aspiration site
There may be other risks depending on your overall health. Talk about any concerns
with your healthcare provider before the procedure.
How do I get ready for a joint aspiration?
-
Your healthcare provider will explain the procedure to you. Ask any questions that
you have about the procedure.
-
You may be asked to sign a consent form. This gives your permission to do the procedure.
Read the form carefully. Ask questions if something is not clear.
-
Tell your healthcare provider if you are sensitive to or are allergic to any medicines,
latex, tape, and anesthetic medicines (local and general).
-
Tell your healthcare provider about all medicines (prescribed and over-the-counter)
and herbal supplements you are taking.
-
Tell your healthcare provider if you have a history of bleeding disorders. Tell them
if you are taking any anticoagulant (blood-thinning) medicines, aspirin, or other
medicines that affect blood clotting. You may need to stop these medicines before
the procedure.
-
If you are or may be pregnant, tell your healthcare provider.
-
Based on your medical condition, your healthcare provider may request other specific
preparation.
What happens during a joint aspiration?
A joint aspiration may be done on an outpatient basis. Or it may be done as part of
your stay in a hospital. Procedures may vary depending on your condition and your
healthcare provider’s practices.
Generally, the procedure follows this process:
-
You may be asked to remove clothing and will be given a medical gown to wear.
-
You will be positioned so that the healthcare provider can easily reach the joint
to be treated.
-
The skin over the joint will be cleaned with an antiseptic solution.
-
If a local anesthetic is used, you will feel a needle prick when it is injected. This
may cause a brief sharp sting.
-
The healthcare provider will insert the needle through the skin into the joint. You
may feel some discomfort or pressure.
-
The healthcare provider will remove the fluid by drawing it into a syringe that is
attached to the needle.
-
The needle will be removed. A sterile bandage or dressing will be applied.
-
The fluid sample may be sent to a lab for examination.
What happens after a joint aspiration?
Once you are home, keep the joint aspiration site clean and dry. Leave the bandage
in place for as long as instructed by your healthcare provider.
The aspiration site may be sore for a few days. Take a pain reliever as advised by
your healthcare provider. Aspirin or some other pain medicines may increase the chance
of bleeding. Be sure to take only approved medicines.
Tell your healthcare provider if you have any of these:
-
Fever of 100.4°F (38°C) or higher, or as directed by your healthcare provider
-
Chills
-
Redness, swelling, bleeding, or other fluid leaking from the aspiration site
-
Increased pain around the aspiration site
Your healthcare provider may give you other instructions after the procedure.
Next steps
Before you agree to the test or the procedure, make sure you know:
-
The name of the test or procedure
-
The reason you are having the test or procedure
-
What results to expect and what they mean
-
The risks and benefits of the test or procedure
-
What the possible side effects or complications are
-
When and where you are to have the test or procedure
-
Who will do the test or procedure and what that person’s qualifications are
-
What would happen if you did not have the test or procedure
-
Any alternative tests or procedures to think about
-
When and how you will get the results
-
Who to call after the test or procedure if you have questions or problems
-
How much you will have to pay for the test or procedure