Arthroplasty
What is arthroplasty?
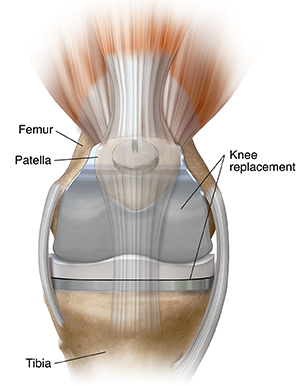
Arthroplasty is a surgery to restore the function of a joint. A joint can be restored
by resurfacing the bones. An artificial joint (prosthesis) may also be used.
Various types of arthritis may affect the joints. Osteoarthritis is the most common
reason for arthroplasty. This is a common degenerative joint disease. It causes a
loss of the cartilage or cushion in a joint.
Why might I need arthroplasty?
Arthroplasty may be used when medical treatments no longer relieve joint pain and
disability. Some treatments for osteoarthritis that may be used before arthroplasty
include:
-
Anti-inflammatory medicines
-
Pain medicines
-
Limiting painful activities
-
Assistive devices for walking, such as a cane
-
Physical therapy
-
Cortisone injections into a knee joint
-
Viscosupplementation injections to add lubrication into the joint. This is to make
joint movement less painful.
-
Loss of excess weight
-
Exercise and conditioning
People who have arthroplasty usually have a lot of relief from their joint pain. They
are more able to do daily activities, and have a better quality of life.
Most joint surgery is done on the hip and knee. Surgery on the ankle, elbow, shoulder,
and fingers is done less often.
There may be other reasons for your healthcare provider to advise arthroplasty.
What are the risks of arthroplasty?
All surgery has risks. The risks of this surgery include:
-
Bleeding
-
Infection
-
Blood clots in the legs or lungs
-
Loosening of prosthetic parts
-
Stiffness or pain that does not go away
Nerves or blood vessels in the area of surgery may be injured. This results in weakness
or numbness. The joint pain may not be relieved by the surgery. Or full function of
the joint may not return.
There may be other risks depending on your overall health. Talk about any concerns
with your healthcare provider before the procedure.
How do I get ready for arthroplasty?
-
Your healthcare provider will explain the procedure to you. Ask any questions that
you have about the procedure.
-
You will be asked to sign a consent form. This gives your permission to do the procedure.
Read the form carefully. Ask questions if something is not clear.
-
Your healthcare provider will ask about your health history. They may also give you
a physical exam. This is done to make sure you are in good health before having the
procedure. You may have blood tests or other diagnostic tests.
-
Tell your healthcare provider if you are sensitive to or are allergic to any medicines,
latex, tape, metals, and anesthesia medicine (local and general).
-
Tell your healthcare provider of all medicines (prescribed and over-the-counter) and
herbal supplements that you are taking.
-
Tell your healthcare provider if you have a history of bleeding disorders or if you
are taking any anticoagulant (blood-thinning) medicines. Tell them if you take aspirin,
or other medicines that affect blood clotting. You may need to stop these medicines
before the procedure.
-
If you are pregnant or may be pregnant, tell your healthcare provider.
-
You will be asked to not eat for about 8 hours before the procedure, generally after
midnight.
-
You may receive a sedative before the procedure to help you relax.
-
You may meet with a physical therapist before your surgery to talk about rehabilitation.
-
Arrange for someone to help around the house for 1 or 2 weeks after you go home from
the hospital.
-
Based on your overall health, your healthcare provider may advise other kinds of preparation.
What happens during arthroplasty?
Arthroplasty may be done as a same day surgery. Or it may need a stay in a hospital.
Ask your healthcare provider about the length of your stay. Procedures may vary depending
on your condition and your healthcare provider's practices.
Arthroplasty may be done while you are asleep under general anesthesia. Or it may
be done while you are awake under local anesthesia. Your anesthesiologist will talk
with you in advance.
Generally, arthroplasty follows this process:
-
You will be asked to remove clothing and will be given a medical gown to wear.
-
An IV line may be started in a vein in your arm or hand.
-
You will be positioned on the operating table in a way that gives the best access
to the joint to be treated.
-
A urinary catheter may be inserted.
-
If there is a lot of hair at the surgical site, it may be shaved off.
-
The anesthesiologist will watch your heart rate, blood pressure, breathing, and blood
oxygen level during the surgery.
-
The skin over the surgical site will be cleaned with an antiseptic solution.
-
The healthcare provider will make an incision in the area of the joint.
-
They will repair or remove the damaged parts of the joint.
-
The incision will be closed with stitches or surgical staples.
-
A sterile bandage or dressing will be applied.
What happens after arthroplasty?
In the hospital
After the surgery, you will be taken to the recovery room for observation. Once your
blood pressure, pulse, and breathing are stable and you are alert, you may be able
to go home. Sometimes you may need to stay overnight at the hospital. If so, you will
be taken to your hospital room.
It is important to begin moving the new joint after surgery. A physical therapist
will meet with you soon after your surgery. They will plan an exercise rehabilitation
program for you. Your pain may be controlled with medicine so that you can take part
in the exercise program. You will be given an exercise plan to follow.
You will go home or to a rehab center. In either case, you will need ongoing physical
therapy until you regain muscle strength and good range of motion.
At home
Once you are home, it will be important to keep the surgical area clean and dry. Your healthcare
provider will give you bathing instructions. The stitches or surgical staples will
be removed during a follow-up office visit.
Take a pain reliever for pain as advised by your healthcare provider. Aspirin or some
other pain medicines may increase the chance of bleeding. Be sure to take only approved
medicines.
Tell your healthcare provider if you have any of these:
-
Fever or chills
-
Redness, swelling, bleeding, or other fluid leaking from the incision site
-
Pain around the incision site that gets worse
-
Numbness or tingling of the affected area
You may go back to your normal diet unless your healthcare provider tells you not
to.
Don't drive until your healthcare provider tells you to. You may be given other activity
limits.
Making some changes to your home may help you during your recovery. These change may
include:
-
Handrails along all stairs
-
Safety handrails in the shower or bath
-
Shower bench or chair
-
Raised toilet seat
-
Stable chair with firm seat cushion and firm back with two arms. This allows your
knees to be lower than your hips when you sit.
-
Long-handled sponge and shower hose
-
Dressing stick
-
Sock aid
-
Long-handled shoe horn
-
Reaching stick to grab objects
-
Firm pillows to raise the hips above the knees when sitting
-
Removing loose carpets and electrical cords that may cause you to trip
Your healthcare provider may give you other instructions after the procedure.
Next steps
Before you agree to the test or procedure make sure you know:
-
The name of the test or procedure
-
The reason you are having the test or procedure
-
What results to expect and what they mean
-
The risks and benefits of the test or procedure
-
What the possible side effects or complications are
-
When and where you are to have the test or procedure
-
Who will do the test or procedure and what that person’s qualifications are
-
What would happen if you did not have the test or procedure
-
Any alternative tests or procedures to think about
-
When and how you will get the results
-
Who to call after the test or procedure if you have questions or problems
-
How much you will have to pay for the test or procedure