Arthroscopy
What is arthroscopy?
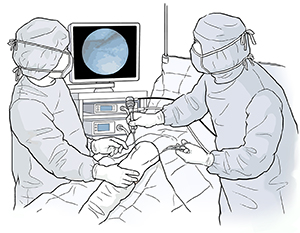
Arthroscopy is a minimally invasive procedure. This means it uses only small incisions.
It's used to diagnose and treat conditions that affect joints. The surgeon can directly
view the inside areas of a joint using a tool called an arthroscope. This is a small,
tube-shaped tool that's used to look inside a joint.
Orthopedic surgeons use arthroscopy to diagnose and treat joint problems. The scope
has a system of lenses, a small video camera, and a light for viewing. The camera
is connected to a video screen. This lets the surgeon see a joint through a very small
incision. The arthroscope is often used along with other tools that are put through
another incision.
Arthroscopy is most often used on the knee. But arthroscopy can be used in other joints.
These include:
-
Shoulder
-
Elbow
-
Ankle
-
Hip
-
Wrist
Why might I need arthroscopy?
Arthroscopy may be used to diagnose and help treat:
-
Inflammation in the knee, shoulder, elbow, wrist, or ankle
-
Shoulder rotator cuff tendon tears
-
Impingement syndrome, which causes pinching of tendons in the shoulder due to squeezing
or rubbing of the rotator cuff and shoulder blade
-
Cartilage damage, such as tears, injury, or wear
-
Ligament tears with instability in the knee
-
Tendon damage
-
Loose bone or cartilage in the knee, shoulder, elbow, ankle, wrist, or hip
Arthroscopy may be used to do a biopsy. It can be used to do corrective surgery. For
example, torn ligaments can be repaired or reconstructed. Arthroscopic surgery may
remove the need for an open surgical procedure.
There may be other reasons for your healthcare provider to advise an arthroscopy.
What are the risks of arthroscopy?
All surgery has risks. The risks of this surgery include:
There may be other risks depending on your overall health. Talk about any concerns
you have with your healthcare provider before the procedure.
How do I get ready for arthroscopy?
-
Your healthcare provider will explain the procedure to you. Ask any questions that
you have about the procedure.
-
You'll be asked to sign a consent form. This gives your permission to do the procedure.
Read the form carefully. Ask questions if something isn't clear.
-
Your provider will ask about your health history. They may give you a physical exam
to make sure that you're in good health before having the procedure. You may have
blood tests or other tests.
-
Tell your provider if you're sensitive to or are allergic to any medicines, latex,
tape, and anesthetic agents (local and general).
-
Tell your provider about all the over-the-counter and prescription medicines and herbal
supplements that you're taking.
-
Tell your provider if you have a history of bleeding disorders or if you're taking
any anticoagulant (blood-thinning) medicines, aspirin, or other medicines that affect
blood clotting. It may be necessary for you to stop these medicines before the procedure.
-
Tell your provider if you're pregnant or think you could be pregnant.
-
You'll be asked to not eat for about 8 hours before the procedure, generally after
midnight.
-
You may receive a sedative before the procedure to help you relax. Because the sedative
may make you drowsy, you'll need to arrange for someone to drive you home.
-
Based on your medical condition, your healthcare provider may give you other instructions
for how to prepare.
What happens during arthroscopy?
Arthroscopy may be done on an outpatient basis. Or it may be done as part of your
stay in a hospital. Procedures may vary depending on your condition and your healthcare
provider's practices. Arthroscopy may be done while you're asleep under general anesthesia.
Or it may be done while you're awake under local anesthesia. The type of anesthesia
will depend on the type of procedure and your overall health. Your anesthesiologist
will talk with you in advance.
Generally, an arthroscopic procedure follows this process:
-
You'll be asked to remove clothing and given a medical gown to wear.
-
An IV (intravenous) line may be put in a vein in your arm or hand.
-
If there's a lot of hair at the surgical site, it may be shaved off.
-
You'll be positioned on an operating table to provide the best access to the joint
to be treated.
-
The anesthesiologist will watch your heart rate, blood pressure, breathing, and blood
oxygen level during the surgery.
-
The skin over the surgical site will be cleaned with an antiseptic solution.
-
The surgeon may drain blood from the surgical area by elevating the extremity and/or
applying an elastic wrap to the extremity. The surgeon may inject a fluid solution,
such as saline, before the arthroscope is inserted. This is done to help expand the
joint.
-
The surgeon will make an incision in the joint area.
-
The arthroscope will be inserted through the incision, into the joint.
-
Other incisions may be made to put other small tools that do grasping, probing, or
cutting.
-
Corrective surgery may be done if needed.
-
The incision will be closed with stitches or adhesive strips.
-
A sterile bandage or dressing will be applied.
What happens after arthroscopy?
After surgery, you'll be taken to the recovery room. Your recovery process will vary
depending on the type of anesthesia you had. The blood flow and feeling in the joint
will be checked. Once your blood pressure, pulse, and breathing are stable and you're
alert, you'll be taken to your hospital room. Or you'll be discharged to go home.
Arthroscopic surgery is usually done on an outpatient basis.
Once you're home, keep the incision site clean and dry. Your healthcare provider will
give you bathing instructions. If stitches are used, they'll be removed during a follow-up
office visit. If adhesive strips are used, they should be kept dry and will fall off
within a few days.
Take a pain reliever for soreness as advised by your provider. Aspirin or some other
pain medicines may increase the chance of bleeding. Be sure to take only approved
medicines.
Limit your activity and the use of the joint for 24 to 48 hours after a diagnostic
arthroscopy. If other procedures are done, such as a ligament repair, your activity
and use of your joint may be limited for a longer period. Your provider will give
you specific instructions. For knee surgery, you may be given an immobilizer to wear.
Your provider may tell you to put ice on the surgical site and to elevate the knee
when you sit.
Tell your healthcare provider if you have any of these:
-
Fever or chills
-
Redness, swelling, bleeding, or other fluid leaking from the incision site
-
Pain around the incision site that gets worse
-
Numbness or tingling in the affected extremity
You may resume your normal diet unless your provider tells you differently.
Your provider may give you other instructions after the procedure.
Next steps
Before you agree to the test or procedure make sure you know:
-
The name of the test or procedure
-
The reason you are having the test or procedure
-
What results to expect and what they mean
-
The risks and benefits of the test or procedure
-
What the possible side effects or complications are
-
When and where you are to have the test or procedure
-
Who will do the test or procedure and what that person’s qualifications are
-
What would happen if you did not have the test or procedure
-
Any alternative tests or procedures to think about
-
When and how you will get the results
-
Who to call after the test or procedure if you have questions or problems
-
How much you will have to pay for the test or procedure