Congenital Heart Defects
What is a congenital heart defect?
A congenital heart defect (CHD) is when the heart or the blood vessels near the heart
don't develop normally before birth.
CHDs occur in about 1 out of 100 babies. Most young people with these conditions are
living into adulthood now. This is due to advances in early diagnoses, testing, treatment,
and surgeries.
In most cases, the cause of a congenital heart defect is unknown. S. The condition
can be passed on through the parents' genes (genetic or hereditary). Some congenital
heart defects are due to alcohol or drug use during pregnancy. A small percentage
of congenital heart defects are related to chromosomal abnormalities.
Most heart defects either cause an abnormal blood flow through the heart, lack of
formation or defect in one of the pumping chambers, or block blood flow in the heart
or vessels. (A blockage is called stenosis and can occur in heart valves, arteries,
or veins.) A hole between 2 chambers of the heart is an example of a very common type
of congenital heart defect.
More rare defects include those in which:
-
The right or left side of the heart is not fully formed (hypoplastic)
-
There is only 1 ventricle
-
Both the pulmonary artery and aorta start from the same ventricle
-
The pulmonary artery and aorta start from the wrong ventricles
Types of congenital heart defects
There are many heart disorders that need clinical care by a healthcare provider. Listed
below are some of these conditions:
Obstructive defects
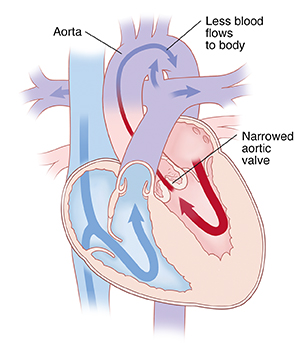
Aortic stenosis (AS)
In this condition, the aortic valve between the left ventricle and the aorta did not
form correctly. It is narrowed. This makes it hard for the heart to pump blood to
the body. A normal valve has 3 leaflets (cusps). But a stenotic valve may have only
1 cusp (unicuspid) or 2 cusps (bicuspid).
In some children, chest pain, abnormal tiredness, dizziness, or fainting may occur.
Otherwise, most children with aortic stenosis have no symptoms. But even mild stenosis
may get worse over time. A catheter-based procedure or surgery may be needed to fix
the blockage. Or the valve may need to be replaced with an artificial or mechanical
one.
Pulmonary stenosis (PS)
The pulmonary valve is located between the right ventricle and the pulmonary artery.
It opens to let blood flow from the right ventricle to the lungs. When a defective
pulmonary valve does not open correctly, the heart has to pump harder than normal
to overcome the blockage. Often the blockage can be corrected by a catheter-based
procedure (balloon valvuloplasty). But some people need open heart surgery.

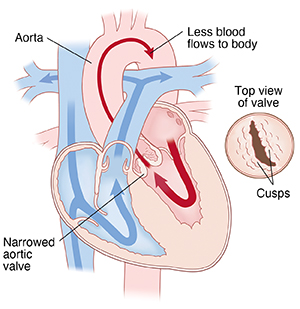
Bicuspid aortic valve
In this condition, a baby is born with a bicuspid valve which has only 2 cusps. (A
normal aortic valve has 3 cusps that open and close). If the valve becomes narrowed,
it's harder for the blood to flow through. Often the blood leaks backward. Symptoms
often don't occur during childhood. But they are often found during the adult years.
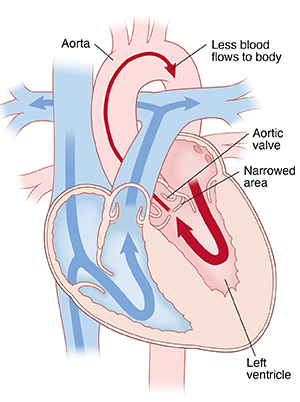
Subaortic stenosis
This condition is a narrowing of the left ventricle just below the aortic valve. Normally,
blood passes through it to go into the aorta. But subaortic stenosis limits the blood
flow out of the left ventricle, often creating an increased workload for the left
ventricle. Subaortic stenosis may be congenital. Or it may be caused by a form of
heart muscle disease (cardiomyopathy).
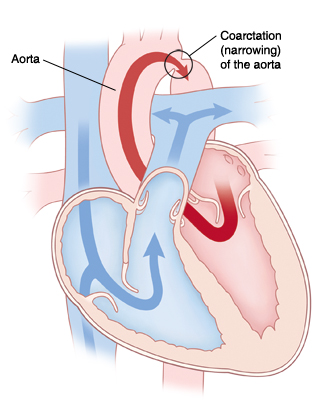
Coarctation of the aorta (COA)
In this condition, the aorta is narrowed (constricted). This blocks blood flow to
the lower part of the body. And it increases blood pressure above the constriction.
Often there are no symptoms at birth. But symptoms can occur as early as the first
week after birth. If severe symptoms of high blood pressure and heart failure develop,
surgery is needed. Less severe cases may not be found until a child is older. But
they can lead to long-term health problems if not fixed.
Septal defects
With some congenital heart defects, a baby is born with an opening in the wall (septum)
that separates the right and left sides of the heart. This lets blood flow between
the right and left chambers of the heart.
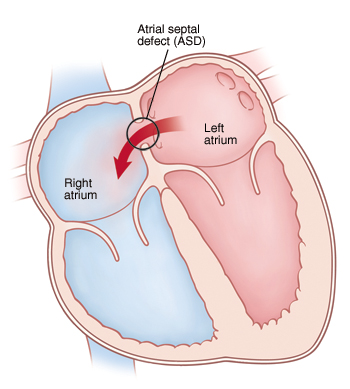
Atrial septal defect (ASD)
In this condition, there is an opening between the 2 upper chambers of the heart (the
right and left atria). This causes abnormal blood flow through the heart. Children
with an ASD have few symptoms. The ASD may be closed by catheter-based methods or
open-heart surgery. Closing the atrial defect in childhood can often prevent serious
problems later in life.
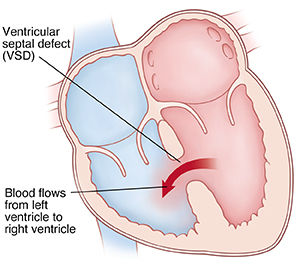
Ventricular septal defect (VSD)
In this condition, there is a hole between the 2 lower chambers of the heart. Because
of this hole, blood from the left ventricle flows into the right ventricle. This is
due to higher pressure in the left ventricle. This causes extra blood to be pumped
into the lungs by the right ventricle. This can create congestion in the lungs. Most
small VSDs close on their own. But larger ones need surgery or a catheter procedure
to fix the hole.
Cyanotic defects
Cyanotic defects are defects in which blood pumped to the body contains less than
normal amounts of oxygen. It causes the skin to turn blue. Infants with cyanosis are
often called blue babies.
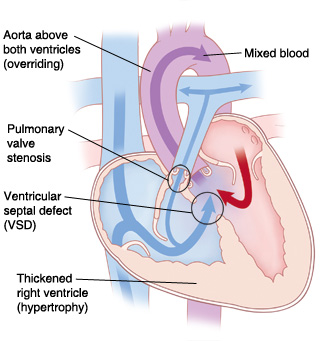
Tetralogy of Fallot
This condition is marked by 4 defects, including:
-
Ventricular septal defect (VSD) which lets blood pass from the right ventricle to
the left ventricle.
-
A narrowing (stenosis) at or above the pulmonary valve. This partly blocks blood flow
from the right side of the heart to the lungs.
-
The right ventricle is more muscular (hypertrophy) than normal.
-
The aorta is directly over the ventricular septal defect.
Tetralogy of Fallot is the most common defect causing cyanosis in people older than
age 2. Most children with tetralogy of Fallot have open heart surgery before school
age (often as babies) to close the VSD and remove the obstructing muscle. Lifelong
medical follow-up is needed.
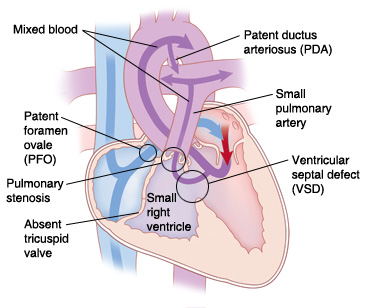
Tricuspid atresia
In this condition, there is no tricuspid valve. So no blood flows from the right atrium
to the right ventricle. This condition is marked by the following:
A surgical shunting procedure is often needed to increase blood flow to the lungs.
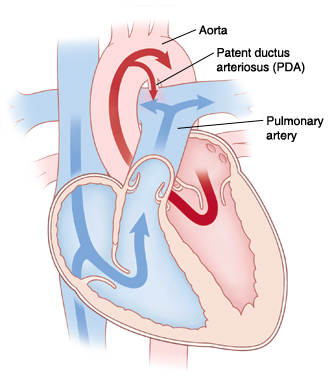
Transposition of the great arteries
In this embryologic defect, the positions of the pulmonary artery and the aorta are
reversed. As a result:
-
The aorta starts from the right ventricle. So the oxygen-poor blood returning to the
heart from the body is pumped back out to the aorta without first going to the lungs
to pick up oxygen.
-
The pulmonary artery starts from the left ventricle. So the oxygen-rich blood returning
from the lungs goes back out to the pulmonary artery and to the lungs again.
Medical care is needed right away to correct this condition.
Other defects
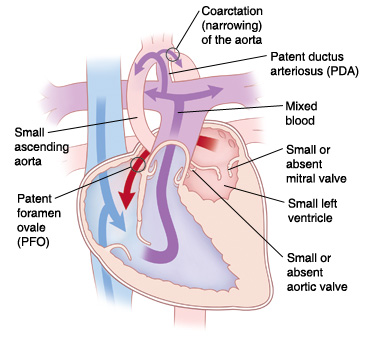
Hypoplastic left heart syndrome (HLHS)
In this condition, the left side of the heart is not fully developed. The left side
includes the aorta, aortic valve, left ventricle, and mitral valve. Blood reaches
the aorta through a hole in a duct called the ductus arteriosus. This opening is called
a patent ductus arteriosus (PDA). A PDA normally closes after birth. But when a child
has HLHS, if the PDA closes, the baby will die. The baby often seems normal at birth,
but the condition will be seen a few days of birth, as the PDA closes. Babies with
HLHS have a gray (ashen) color, have little or no pulse in their legs, have trouble
breathing, and can't feed. Treatment is surgical. Often a series of 3 surgeries is
needed.
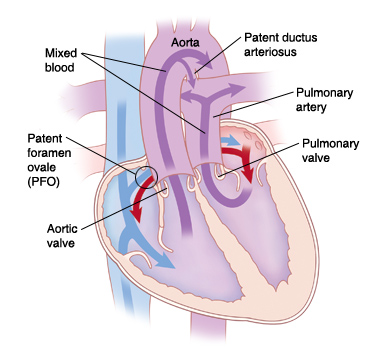
Patent ductus arteriosus (PDA)
This condition occurs when the PDA doesn't close normally after birth. This allows blood
to mix between the pulmonary artery and the aorta. When it doesn't close, extra blood
may flood the lungs and cause pulmonary congestion. PDA is often seen in premature
babies.
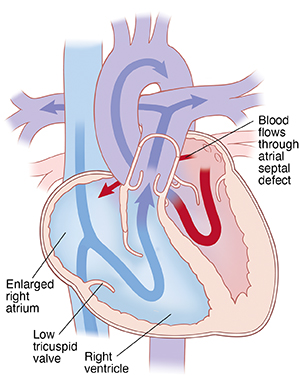
Ebstein anomaly
In this defect, there is a downward displacement of the tricuspid valve (located between
the upper and lower chambers on the right side of the heart) into the right bottom
chamber of the heart (right ventricle). This leads to an enlarged atrium. That can
cause rhythm abnormalities and heart failure. It's often linked to an atrial septal
defect.
Who treats congenital heart defects?
For young children
Babies with congenital heart problems are followed by specialists called pediatric
cardiologists. These healthcare providers diagnose heart defects and help manage a
child's health before and after surgery to fix the heart problem. Specialists who
correct heart problems in the operating room are pediatric cardiovascular or cardiothoracic
surgeons.
For adults
To achieve and keep the highest possible level of wellness, it's vital that people
born with CHD who have reached adulthood transition to the appropriate type of cardiac
care. The type of care needed is based on the type of CHD a person has. People with
simple CHD can often be cared for by a community adult cardiologist. People with more
complex types of CHD will need to be cared for at a center that specializes in adult
CHD.
Adults with CHD need guidance to plan for key life concerns, such as:
Transitioning from pediatric care to adult care
The transition to adult care can start in your child's early teen years. It should
be personalized for your child. Early on, you and the specialist should talk with
your young teen about the idea that they will one day be responsible for their own
care. This will depend on several factors, such as your child's ability to care for
themselves. It's best started when your child is fairly healthy. Your child will need
to be able to:
A successful transition to adult care will review:
Talk with the pediatric cardiologist about how to make sure of a smooth transition
from pediatric to adult care for your child. This can help your child
-
Ask their advice about finding qualified healthcare providers.
-
Plan for changes in insurance.
-
Understand the psychological challenges that can occur with teens when transitioning
to an adult practice. These include nervousness, excitement, hope, and frustration.
-
If possible, your teen should have someone other than a family member to discuss impacts
of their disease on dating and other social relationships.
-
Work with your child's pediatric clinic to make a list of goals for transition. Check
in on these goals at each routine visit.
Talk with your child early and often about their role as a patient. Having your child
take a greater role in their own healthcare over time is a big responsibility. Give
your child positive reinforcement when they show independence in their own healthcare.