Right Heart Catheterization
What is right heart catheterization?
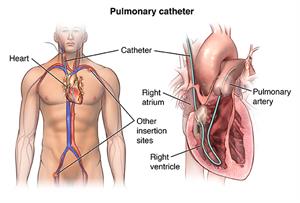
Your healthcare provider may do a right heart catheterization (cath) to see how well
or poorly your heart is pumping, and to measure the pressures in your heart and lungs.
This test is also known as a pulmonary artery catheterization.
In a right heart cath, your healthcare provider guides a small, hollow tube called
a pulmonary artery (PA) catheter to the right side of your heart. They then pass the
tube into your pulmonary artery. This is the main artery that carries blood to your
lungs. Your healthcare provider observes blood flow through your heart and measures
the pressures inside your heart and lungs.
As the catheter advances toward your pulmonary artery, your healthcare provider measures
pressures along the way, inside the chambers on the right side of your heart. This
includes the right atrium and right ventricle. Your healthcare provider can also take
indirect measurements of pressures on the left side of your heart. Your cardiac output—the
amount of blood your heart pumps per minute—is also determined during a right heart
cath. All of these measurements are used to diagnose heart conditions and to determine
what treatment is right for you.
In some cases, you get IV (intravenous) heart medicine during a right heart cath to
see how your heart responds. For example, if the pressure in your pulmonary artery
is high, your healthcare provider will give you medicine to dilate, or relax, the
blood vessels in your lungs and lower the pressures. A healthcare provider will take
several pressure measurements during the procedure to assess your body's response
to the medicines.
If output from your heart is low or the pressures in your heart and lungs are too
high, your provider will leave the PA catheter in place. This is to watch the effects
of different IV medicines. You will most likely be monitored in the intensive care
unit (ICU) in this case. This lets your providers find the best treatment to improve
your heart's function.
Why might I need a right heart cath?
You might need a right heart cath to diagnose or manage the following conditions:
-
Heart failure. A condition in which your heart muscle has become so weak that it can't pump blood
efficiently. This causes fluid buildup (congestion) in your blood vessels and lungs.
Fluid may also build up in your feet, ankles, and other parts of your body.
-
Shock. This causes reduced flow of blood and oxygen to the tissues of your body. Sudden
onset of heart failure, severe bacterial infection in your bloodstream (sepsis), or
severe blood loss (hemorrhagic) can cause shock.
-
Congenital heart disease. These are birth defects that develop in the heart. An example is ventricular septal
defect. This is a hole in the wall between the lower chambers of your heart.
-
Heart valve disease. Malfunction in one or more of your heart valves may interfere with normal blood flow
within your heart.
-
Cardiomyopathy. This is an enlargement of your heart due to thickening or weakening of your heart
muscle. It can eventually lead to heart failure.
-
Pulmonary hypertension. This is increased pressures in the blood vessels in your lungs. It can lead to trouble breathing
and right-sided heart failure.
-
Heart transplant. With a heart transplant, a right heart cath is done before the heart transplant and
also helps measure the function of the transplanted heart. It also allows a healthcare
provider to take a biopsy to make sure the transplanted heart is not being rejected.
Your healthcare provider may have other reasons to advise a right heart cath with
biopsy.
What are the risks of right heart cath?
Possible risks of right heart cath include:
Other, rare complications may include:
-
Abnormal heart rhythms, such as ventricular tachycardia (fast heart rate in your lower
heart chambers)
-
Cardiac tamponade (fluid buildup around your heart that affects its ability to pump
blood effectively), rarely resulting in death
-
Infection
-
Air embolism (air leaking into your heart or chest area), rarely resulting in death
-
Blood clots at the tip of the catheter that can block blood flow
-
Pulmonary artery rupture. This is damage to the main artery in your lung. This can
cause serious bleeding. It may need chest surgery to correct.
For some people, having to lie still on the cardiac cath table for the whole procedure
may cause some discomfort or back pain. You will be given medicine to help you relax.
There may be other risks, depending on your specific condition. Be sure to discuss
any concerns with your healthcare provider before the procedure.
How do I get ready for a right heart cath?
Your healthcare provider will explain the procedure and you can ask questions.
-
You will be asked to sign a consent form that gives your permission to do the test.
Read the form carefully and ask questions if something is not clear.
-
Tell your healthcare provider if you are sensitive or allergic to any medicines, latex,
tape, sleep and numbing medicine, or local and general anesthesia.
-
Tell your provider if you are pregnant or think you could be pregnant.
-
Tell your provider of all medicines (prescription and over-the-counter), vitamins,
and herbal supplements you are taking.
-
Tell your provider if you have a history of bleeding disorders, or if you are taking
any anticoagulant (blood-thinning) medicines. These may include warfarin, aspirin,
or other medicines that affect blood clotting. You may be told to stop some of these
medicines before the procedure.
-
Tell your provider if you have a pacemaker or an implantable defibrillator.
-
If you have an artificial heart valve, your healthcare provider will decide if you
should stop taking warfarin before the procedure.
-
Follow all directions you are given for not eating or drinking before the procedure.
-
If the insertion site is in your groin, the area around your groin may be shaved.
Based on your condition, your provider may ask for other specific preparation.
What happens during a right heart cath?
Your healthcare provider will do your right heart cath in the cardiac cath lab. If
you are critically ill, the procedure may take place in the ICU. The procedure may
be done on an outpatient basis, or as part of your hospital stay. The procedure may
vary depending on your condition and your healthcare provider's practices.
-
You will need to remove any jewelry or other objects that may interfere with the procedure.
You may wear your dentures or hearing aids if you use either of these.
-
You will change into a hospital gown and empty your bladder.
-
A healthcare professional will start an IV line in your hand or arm before the procedure
for injection of medicine and to give IV fluids, if needed.
-
You will lie on your back on the procedure table.
-
A healthcare professional will connect you to an electrocardiogram monitor. This machine
records the electrical activity of your heart during the procedure using small, adhesive
electrodes. Healthcare providers will watch your vital signs during the procedure.
These are your heart rate, blood pressure, breathing rate, and oxygen level.
-
Your healthcare provider will give you a mild sedative to help you relax, but you
will not be put to sleep.
-
Sterile towels will be placed over your chest and neck if your neck vein is used.
-
If your groin is used, sterile towels will be placed over your groin area.
-
Your provider will clean and numb the skin over your neck or groin with a local anesthetic.
A small needle will be used to find your vein. Then your provider will insert a thin
tube called a catheter into your vein. You may feel some burning or stinging when
the numbing medicine is given. There may be some pressure as the needle punctures
your vein.
-
Your provider will place an introducer sheath (a slightly larger, hollow tube) into
your vein first, and will then insert the PA catheter through the introducer. You
may feel some pressure as the introducer is placed. Once the PA catheter is in place,
your heart pressures will be measured.
-
`Depending on where the procedure is done and for what reasons, the provider may use
X-ray images to guide the catheter to the correct area.
-
IV heart medicine may also be given to evaluate your heart's response. It may take
about 30 minutes to keep track of your heart's response to the medicine.
-
Once your provider gets all the information they need, your medical team will remove
the catheter and introducer. But if the team thinks you need more monitoring, these
will stay in and you will stay in the ICU.
What happens after a right heart cath?
A member of the medical staff will put pressure over your insertion site for about
5 to 10 minutes to make sure you are not bleeding. Or they may use a closure device
over the insertion site.
If your neck vein was used (most common), you can sit up comfortably. If a groin vein
was used for the procedure, you will have to lie flat in bed for a few hours so the
puncture site can heal correctly.
You can eat and drink normally after the procedure. The nurse will watch the insertion
site for bleeding and check your blood pressure, heart rate, and breathing while you
recover. Let the nurse know if you have any chest pain or trouble breathing.
Your healthcare provider will discuss the findings of the right heart cath and plans
for treatment, if needed. Most of the time, you will be able to go home a few hours
after the procedure.
Once at home, watch the insertion site for bleeding, abnormal pain, swelling, and
abnormal discoloration or temperature change at or near the insertion site. A small
bruise is normal. If you notice a constant or large amount of blood at the site that
can't be contained with a small bandage or dressing, call your healthcare provider.
It will be important to keep the insertion site clean and dry. Your provider will
give you specific bathing instructions.
Your healthcare provider may advise you not to do any strenuous activities. They will
tell you when you can return to work and resume normal activities.
Call your healthcare provider to report any of the following:
-
Shortness of breath or trouble breathing
-
Fever of 100.4 °F (38°C) or higher, or as advised by your provider
-
Chills
-
Increased pain, redness, swelling, or bleeding or other drainage from the insertion
site
-
Coolness, numbness or tingling, or other changes in the affected extremity
-
Chest pain or pressure, nausea or vomiting, profuse sweating, dizziness, or fainting
Your healthcare provider may give you other instructions after the procedure, depending
on your situation.
Next steps
Before you agree to the test or procedure, make sure you know:
-
The name of the test or procedure
-
The reason you are having the test or procedure
-
What results to expect and what they mean
-
The risks and benefits of the test or procedure
-
What the possible side effects or complications are
-
When and where you are to have the test or procedure
-
Who will do the test or procedure and what that person’s qualifications are
-
What would happen if you did not have the test or procedure
-
Any alternative tests or procedures to think about
-
When and how you will get the results
-
Who to call after the test or procedure if you have questions or problems
-
How much you will have to pay for the test or procedure