Pediatric Critical Care

High Quality & Coordinated Care
The Pediatric Critical Care Division at Golisano Children's Hospital is dedicated exclusively to the specialized care of infants, children and young adults with serious illnesses, injuries and peri-operative needs. This is the largest intensive care service for children in Upstate New York. Specialized care is provided 24/7 by nationally recognized pediatric intensivists, pediatric cardiac intensivists, pediatric critical care advanced practice providers, nurses, and respiratory therapist.
The Pediatric Intensive Care Unit (PICU) and the Pediatric Cardiac Care Center (PCCC) are physically located next to each other allowing specialists and services to be shared and readily available should your child need them. In addition, they are positioned between the inpatient floors and the operating rooms shortening transport times and reducing risks for our patients.
Support for Our Patients & Families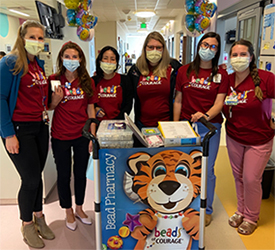
We are proud to provide the Beads of Courage® Cardiac Program at Golisano Children’s Hospital. The program is a program of Beads of Courage, Inc. dba Center for Arts in Nursing, whose mission is to provide innovative arts in medicine programs for children coping with serious illness, their families, and the clinicians who care for them. Beads of Courage® is a federally registered trademark of Beads of Courage, Inc., and is used under license. For more information on Beads of Courage®, visit: www.beadsofcourage.org.
Advanced Technology
We are now treating infants who are critically ill and renal failure with a new tool that is built to improve the outcomes for the most fragile patients. The Cardio-Renal Pediatric Dialysis Emergency Machine (CARPEDIEM TM) is a new continuous renal replacement therapy (CRRT) designed specifically for small infants with acute kidney injury or kidney failure requiring dialysis. With 3 CARPEDIEM’s, Golisano Children’s Hospital is only the second hospital in the country to be trained and proficient in treating patients with the device.
Pediatric Intensive Care Unit

The Pediatric Intensive Care Unit (PICU) is a 12-bed unit providing intensive care to critically ill and injured infants, children and young adults, generally ranging from newborn to 19 years.
Pediatric Cardiac Care Center

The Pediatric Cardiac Care Center (PCCC) provides care for neonates and young adults with acquired and congenital heart disease, rhythm disturbances, and other cardiac related conditions.
Part of Strong Memorial Hospital