News from Pediatrics
News from Pediatrics
Meet Golisano’s Pediatric Chaplain, Rev. Patti Blaine
Tuesday, December 13, 2022

Hometown: Grew up in Vestal, NY. My husband, daughter, and I moved to Rochester from Woodside, Queens in 2006.
Education/Background: Graduate of Colgate Rochester Crozer Divinity School with an M.A. in Religious Studies and certification in Anglican Studies. She is ordained as a deacon in the Episcopal Church.
Rev. Patti Blaine is the pediatric chaplain for URMC, providing support to patients and families at Golisano Children’s Hospital. She took this role in September 2022 and, shares more about her work.
Q. What would you like patients and families to know about your role?
A. I provide emotional as well as spiritual support to people of all religious traditions—and none! Some of the work I’m proudest of has been companioning others through terrible, heartbreaking situations, normalizing their emotions, listening reflectively, exploring their spiritual and existential questions and occasionally providing prayer in their religious tradition when asked.
Q. What do you enjoy most about your work?
A. There’s an item in the chaplaincy flowsheet I love to click: Shared play. Coming alongside children or adults, and being playful by looking at art, listening to music, watching a movie or playing a game often opens deep spiritual insight into what the patient, family member, or staff is really worried about and hoping for.
Q. What’s the most difficult part of your work?
A. The generational and grinding effects of poverty and racial inequity are laid bare in the hospital setting. From the carnage of violence in the trauma bays to the drug-addicted newborn in the NICU, from chronic cases of diabetes on dialysis to children who’ve met a pediatrician too late to cure their cancer, these social ills wear on me. I cope by focusing on the individual and doing my best to provide unconditional positive regard.
Q. Favorite hobby outside of work?
A. This question is easy! Knitting. I often say that I’m going home to “knit myself back together” at the end of a long and difficult shift. And I’m not kidding! Being present to the pattern and color of the work, the susurration of the sliding needles, the flow of the yarn between my fingers—knitting heals me.
Q. The holidays can be tough for a lot of people—especially if they find themselves at the hospital. What’s one piece of advice you can offer them?
A. Remember that this is a season, one out of many that make up our lives. While we’re in it, it overwhelms us with grief, loneliness, desperation, etc. I know this all too well. Try to recall the love and joy that came before. Try to imagine one day, when this season is over, some of or maybe all that love and joy will return. When it does, it may be bittersweet, tinged with the color of this time, but it will be. And, although it feels completely otherwise, you are not alone in this experience.
URMC’s Golisano Children’s Hospital Receives Level 1 Pediatric Trauma Center Designation
Wednesday, September 28, 2022
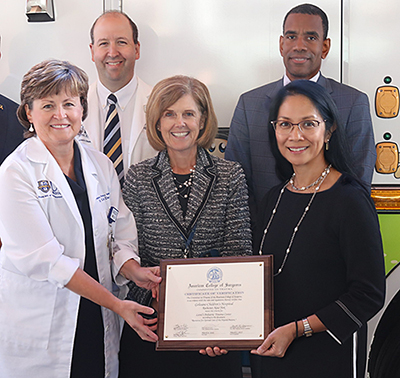
UR Medicine Golisano Children’s Hospital (GCH) has been designated as a Level 1 Pediatric Trauma Center by the American College of Surgeons and New York State, the highest possible classification for trauma care and evidence that GCH is delivering best-practice treatment, education, and research in the field.
Earning this classification was part of a multi-year process in which GCH increased its staffing and facilities infrastructure, including the addition of several pediatric surgeons as well as dedicated staff for Quality Improvement (QI) – a process that streamlines operations and tracks results. Level 1 classification also represents the expansion of GCH services that has been in process the past decade - including the construction of the dedicated GCH hospital facility in 2015 – and offers a roadmap for GCH to continue to offer new, innovative trauma care in the region.
“Level 1 means the care we’re giving is of the highest quality and there’s no form of medical treatment in which we’d need to transfer a patient,” said Marjorie Arca, M.D., chair of the Department of Pediatric Surgery. “This allows for a more comprehensive care team and releases the burden on families who no longer have to fear of traveling and can focus fully on the recovery of their child.”
Level 1 classification means that GCH is now certified to provide the following services and expertise:
- 24-hour coverage by general surgeons, and prompt availability of care in specialties such as orthopedic surgery, neurosurgery, anesthesiology, emergency medicine, radiology, internal medicine, plastic surgery, oral and maxillofacial, pediatric and critical care.
- Primary referral resource for communities in nearby regions.
- Provide leadership in prevention and public education to surrounding communities.
- Provide continuing education of the trauma team members.
- Incorporate a comprehensive quality assessment program.
- Operate an organized teaching and research effort to help direct new innovations in trauma care.
- Offer Programs for substance abuse screening and patient intervention.
- Meet minimum requirements for annual volume of severely injured patients.
In a national environment where youth gun violence is soaring, the Level 1 classification means that GCH is able to provide both life-saving treatment to victims and offer public education to communities and patient intervention to prevent recidivism.
“We try not just to talk to the patient, but find out what’s impacting the person behind the trauma, and work to utilize resources such as social work and child life to keep children out of the hospital and from experiencing non-accidental trauma,” said Arca.
Level 1 classification will also allow GCH to expand its research and education for nursing and trauma team members. This research effort is growing monthly and contributing to the overall wealth of knowledge on how to best care for injured children.
“Being Level 1 isn’t just about the quality of treatment,” said Derek Wakeman, M.D., pediatric surgeon. “It’s a recognition of the strength of our research into improving care and being a regional leader in providing outreach and education to all of the nurses in the hospital as well as EMS caregivers in the community.”
Going forward, the GCH trauma team will conduct continuous evaluations to drive quality improvement. Additionally, multiple teaching efforts - such as special certification and simulations with residents, nurses and the emergency department – will help develop the highest level of skill-set in the operating rooms at GCH at all times.
“Earning the Level 1 Pediatric Trauma Center designation for UR Medicine Golisano Children’s Hospital is not only an incredible feat for our community, but one for our staff,” said Mark Gestring, M.D., professor of surgery and chief of Emergency Medicine at the University of Rochester Medical Center. “Our teams work tirelessly to be sure that every resource is available in our trauma center and that we are able to serve any child that comes through our doors, no matter the injury, all while keeping them here in Rochester. It’s a distinction that we are honored to receive and will strive to maintain.”
Phil Davidson: Trailblazer for Children with Intellectual and Development Disabilities
Wednesday, April 6, 2022
Phil Davidson, Ph.D., passed away on Thursday, February 10th, 2022. A long-time faculty member and professor emeritus of Pediatrics, Environmental Medicine and Psychiatry and former Director of the Strong Center for Developmental Disabilities at URMC, Davidson was a tireless advocate who played a substantial role in recognizing the health needs of people with intellectual and developmental disabilities across the lifespan, integrated behavioral health, and disability rights. In addition, he helped develop specialty clinics for assessment and care in Developmental-Behavioral Pediatrics, IDD-related research at URMC, and focused education for trainees on IDD.
“Phil Davidson wore many hats in his long career – clinical psychologist, community advocate, educator and researcher,” said Dr. Susan Hyman, M.D., professor of Pediatrics and division chief of Developmental and Behavioral Pediatrics (SMD). “His career at URMC paralleled the advances in recognition and care for individuals with IDD nationally. He was there as a champion each step of the way.”
Phil was the Initial Director of both the Leadership Education in Neurodevelopmental Disabilities (LEND) program – which offers which offers collaborative interdisciplinary training to prepare professionals for advocacy for individuals with neurodevelopmental disabilities in medical and nonmedical systems - and the Strong Center for Developmental Disabilities, the University Center for Excellence in Developmental Disabilities (UCEDD) that promoted the growth of interest in employment and health equity for individuals with neurodevelopmental disabilities here in Rochester as well as the Division Chief of what is now Developmental and Behavioral Pediatrics.
First awarded in 1977, the UCEDD collaborates with the community of people with disabilities and their families to create a world in which people of all ages with intellectual and developmental disabilities are valued and respected, lead self-determined lives in the community of their choice, and have the opportunity to contribute to that community and society at large.
In addition to his leadership roles at URMC, Davidson served at the President of International Association for the Scientific Study of Intellectual and Developmental Disabilities (IASSIDD), the largest and oldest scientific organization of its kind in the world that promotes worldwide research and exchange of information on intellectual and developmental disabilities.
“His last accolade – the presidency of IASSID – was a fitting recognition of his stature in the field,” said Hyman.
Last year Davidson published a book in collaboration with Hyman – A History of Developmental and Behavioral Pediatrics at the University of Rochester – that served as culmination of his accomplishments at URMC. During his 45-year tenure, Davidson was the supervisor for more than 50 postdoctoral fellows in pediatric psychology and predoctoral fellows in clinical psychology, and across his career, he published 177 journal articles, and 46 books/chapters.
Davidson is survived by his wife of 55 years, Margaret B. Davidson of Hilton Head Island, SC, his sons Andrew Davidson of West Chester, PA, and Alec Davidson of Marietta, GA, their wives, Carolyn and Laura, and 4 grandchildren: Jack 18, Emma 14, Luca, 17, and Nico, 13.
New Initiative Will Offer Obesity Counseling for Families
Friday, April 1, 2022

Children who are struggling with obesity will have an opportunity to participate in a new family-focused counseling program in select pediatric clinics led by the University of Rochester Medical Center (URMC) in the Monroe County region.
Family walking on a country pathCalled TEAM UP, the program is a weight management study focused on getting families healthier in four states – New York, Missouri, Illinois and Louisiana. The purpose of this research project is to test different ways to help children and their families lose weight through healthy eating and physical activity.
The program include two components: counseling by a primary care provider focusing on healthy eating and activity habits, and a combination of provider counseling and family-based behavioral treatment for children and parents. The program will run through the end of 2023.
Childhood obesity is a growing public health crisis, and the pandemic has only exacerbated this issue as more children stayed home and physical activity was restricted in the early days of COVID-19.
“This is a program that addresses a need that has been building for more than a decade,” said Stephen Cook, M.D., M.P.H., associate professor in the Department of Pediatrics at URMC. “Obesity is one of the most common chronic conditions for families and has gotten worse during the pandemic.”
Technology will be a key component of TEAM UP. Applications will track data on physical activity and eating habits, and families will be to participate in counseling sessions through Zoom. “A byproduct of the pandemic is that we found out that Zoom visits made the program more feasible and accessible,” said Cook.
Obesity is one of the most common chronic conditions for families and it's gotten worse during the pandemic.”
– Stephen Cook, M.D., M.P.H.
While many virtual programs have drawbacks in comparison to in-person services, obesity counseling may be better suited for remote implementation due to increased comfort and convenience for families, according to Cook.
“There can be a stigma and shame with obesity,” he said, “often times parents don’t want to go to the weight station at the doctor’s office. In addition, since this program pairs parents and children, there’s less pressure to coordinate schedules to make it to the doctor’s office.”
Family participation will be an important component of TEAM UP, as research has shown that a collective effort is the most effective method to address child obesity. “Obesity is not a personal choice,” Cook says. “Changes can’t be left to the individual, it has to involve the whole family.”
This collective approach has to start as early as possible once the problem has been identified by the pediatrician. Family-wide interventions recommended by TEAM UP counselors could include reducing exposure to screens and spending more time outside, limiting fast food, and engaging in more meal planning. “We find better results with kids when we also see results with parents.”
The following pediatric practices will be participating in the TEAM Up program:
- Brighton Pediatrics
- Elmwood Pediatrics
- Fairport Pediatrics
- Finger Lakes Medical Associates
- Highland Family Medicine
- Irondequoit Pediatrics
- Lewis Pediatrics
- Mendon Pediatrics
- Oak Orchard Health
- Pathway Pediatrics – Trillium Health
- Rochester General Pediatric Associates
- Westside Pediatrics
- UR Medicine Primary Care – North Greece
- UR Medicine Primary Care – Westfall Pediatrics
Families interested in participating in the program are encouraged to contact the pediatric practices listed above if they are a patient. More practices are expected to be added in the coming months.
Pediatric Emergency Department Chief Wins Rochester ATHENA Award
Monday, March 21, 2022

Ever since she was a young child, Colleen Davis, M.D., M.P.H., chief of Pediatric Emergency Medicine at Golisano Children’s Hospital, knew that she wanted to be a doctor.
Growing up in Binghamton, NY, Davis’s father was the police chief and her mother was a telephone operator. Although no one in her large extended family was a doctor, Davis knew she wanted to be a physician and her parents encouraged her to shoot for the stars, telling her she could ‘be whatever she wanted to be’. This constant encouragement - coupled with the young Davis’s aptitude for the sciences - motivated her to take every opportunity she could to immerse herself in medicine.
“The more I shadowed or volunteered to work with physicians, the more I loved it,” said Davis.
Davis has channeled that initial spark of interest into a career of excellence, and on January 20th, she was recognized as the ATHENA Award winner at the 36th annual ATHENA International Awards, hosted by the Greater Rochester Chamber of Commerce at the Rochester Riverside Convention Center.
Established in 1982, The ATHENA International Award is given to a professional female leader who has demonstrated significant achievements in business, community service, and the professional advancement of women. Davis was honored for her leadership, both for managing the highly-demanding environment of the Pediatric Emergency Department (Ped ED) and her mentorship of young trainees.
"It's a tremendous honor, and I am humbled to have been selected for this award,” said Davis.
After graduating in 1986 from Upstate Medical School in Syracuse, Davis moved to Rochester for residency training at the University of Rochester Medical Center (URMC), where she also earned a Masters of Public Health. For 31 years, she has worked at URMC/GCH, providing emergency treatment for children in the greater Rochester community. Davis cares for a variety of patients in the ED, from children with common illnesses such as fever, asthma and broken bones to those with life threatening conditions including meningitis and major trauma.
This accessibility – serving all types of patients from all walks of life – is a primary reason Davis was drawn to emergency medicine.
“In Emergency Medicine, we’re the safety net and I like that. We’re open 24/7, and we never turn anyone away, she said. We see anyone - for anything - at any time.”
Since 2007, Davis has served as chief of the Pediatric ED. The role requires operational and administrative leadership in a fast-paced, high acuity environment. In addition, Davis has published several medical articles and presented her work nationally.
During her 15 years as chief, Davis has guided the emergency department with a steady hand, most recently through the COVID pandemic, which has strained emergency departments across the country. During intense periods, Davis emphasizes a mantra shared by Michael Kamali, M.D., chair of the Department of Emergency Medicine: one patient at a time.
“We have a team approach, and our team can be very nimble. We’re able to flex up and flex down when the situation demands and take each patient as they come,” she said.
In addition to managing the clinical operations, Davis - along with many other faculty members - has overseen the clinical education of trainees in the ED. For Davis, this training is uniquely rewarding because “by teaching young physicians we are building the foundation for the next generation of medicine”. Many of Davis’s former subspecialty fellow trainees have gone on to lead Pediatric Emergency Departments across the country.
"As a 4th year medical student, in 2003, I was lucky enough to be granted a month long elective in the Pediatric ED at URMC. I remember introducing myself, Colleen stopping what she was doing, saying ‘sit down, tell me about yourself and welcome to our ED,’ said Elizabeth Murray, D.O., faculty director of Child Health and Safety Communications at GCH. “I shared with her my interest in specializing in Pediatric Emergency Medicine, hence my excitement with being able to land this rotation. From that moment on, Colleen was there to ensure I had what I needed, met the people I needed to meet to further my goals, and had all the support needed to go through the cumbersome application process."
In addition to her work in the medical center, Davis is active in the entire University as a member of the Faculty Senate, Commission on Women and Gender Equality and a number of Presidential advisory committees. Davis has supported Our Lady of Mercy School for Young Women for 16 years. She is the parent of three Mercy graduates: ’12, ’15, ’18 and is a current member of the OLM Board of Trustees, Academic-Student Affairs and Covid Advisory Committees.
“For more than three decades, Colleen has been there for children and families in our region providing top-quality emergency care and leadership,” said Patrick Brophy, M.D., physician-in-chief at Golisano Children’s Hospital, “she’s a model for our community and there’s nobody more deserving of this honor.”
Abbott Formula Recall
Monday, February 21, 2022
On February 17, 2022, Abbott Nutrition announced a voluntary recall of certain powdered infant formula products manufactured at one of their plants.
Brands impacted include Similac, Alimentum, and EleCare.
- For the latest information on this recall, please visit the FDA website. FDA Warns Consumers Not to Use Certain Powdered Infant Formula Produced in Abbott Nutrition’s Facility in Sturgis, Michigan | FDA
- Abbott Voluntarily Recalls Powder Formulas Manufactured at One Plant