Radiation Oncology
What Is Radiation Oncology?
 Radiation oncology is one of the three major cancer specialties in oncologic medicine. It uses energy from radiation beams, radio isotopes, or charged particles to target tumors and to eradicate cancer cells.
Radiation oncology is one of the three major cancer specialties in oncologic medicine. It uses energy from radiation beams, radio isotopes, or charged particles to target tumors and to eradicate cancer cells.
Radiation beams are usually generated in treatment machines, such as linear accelerators or high-energy CT scanners. Another type of radiation treatment uses radioisotopes, or radioactive materials. These are utilized in radiation implants and radioisotope-labeled molecules in the treatment of various cancers.
In addition to getting rid of cancer, radiation treatment is highly effective in reducing symptoms such as cancer-related pain. Radiation has also been used in the treatment of many benign (non-cancerous) conditions in both adults and children.
What Makes URMC Different?
At the Wilmot Cancer Center, Radiation Oncology is an essential part of multidisciplinary care. A team of experts from surgery, medical oncology, radiation oncology, and many other disciplines will come together to evaluate and manage your cancer treatment. This is a unique approach to care and is considered the ideal model of cancer care. You should feel remarkably confident in coming to URMC, the region’s leader in radiation oncology.
We provide state-of-the-art treatment technology to increase the curability of cancer while reducing side effects. Our comprehensive cancer care team includes physician radiation oncologists, radiation physicists, radiation therapists, dosimetrists, nurses, social workers, and nutritionists.
What Should I Expect as a Patient?
A radiation oncologist will direct the radiation treatment process and plans. Your team will also include a secretary, a nurse, a nurse practitioner, a resident physician in training, radiation therapists who operate the treatment machines, and a radiation dosimetrist or physicist specializing in radiation treatment physical plans.
The department also offers assistance from social workers and nutritionists. Support groups for cancer patients are also available. These include disease-specific groups, age-specific groups, and many others.
A typical radiation treatment process begins with an initial consultation with your radiation oncologist. The treatment recommendation, indication, rationale, benefits, side effects, and potential risks will be explained to you. This is followed by a radiation simulation session, which takes approximately one hour. This simulation process ensures the accuracy of your treatment plan.
Your actual treatment will begin 7-14 days later. However, patients with cancer-related emergencies can begin their treatments sooner. Daily treatment visits may take 15 -30 minutes and generally last 1 to 8 weeks, depending on the diagnosis and the treatment plan. The stereotactic brain radiosurgery is generally completed in one session. The stereotactic body radiosurgery is generally completed in less than 10 sessions.
Your radiation oncologist, therapists, and the team nurse will be there for you every step of the way. They will help you assess treatment-related side effects, your progress, and tolerance.
What Technology Do You Offer?
We offer state-of-the-art equipment for external beam radiation at Strong Memorial Hospital (SMH), Highland Hospital (HH), Cancer Center at Greece, and Sands Cancer Center.
- CT simulators (SMH, Greece)
- Megavoltage CT (SMH)
- Cone-beam CT units (SMH)
- Linear accelerators with IMRT and IGRT capabilities (SMH, HH, Greece, Sands)
- Novalis Radiosurgery (SMH)
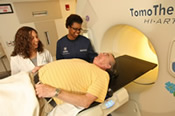
- TomoTherapy (SMH)
- Total Body Irradiation (SMH)
- Lutathera (lutetium Lu 177 dotatate) PRRT (Peptide Receptor Radionuclide Therapy) for patients with neuroendocrine tumors (Dr. Qiu at SMH 585-275-5625)